Lancet:年龄与劲动脉内膜切除术和支架置入术后的卒中及死亡风险的关系
2016-02-13 MedSci MedSci原创
原始出处:George Howard, Prof Gary S Roubin, et al,Association between age and risk of stroke or death from carotid endarterectomy and carotid stenting: a meta-analysis of pooled patient data from fo
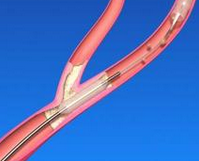
背景:四个随机对照试验比较了颈动脉支架植入(CAS)和颈动脉内膜切除手术(CEA),发现年龄是重要的效应修饰因子,在年龄较轻的患者中CEA结局比CAS的结局要好。我们旨在描述年龄对于有症状患者的治疗差异并评估特定年龄段狭窄(5年)人群的卒中和死亡风险。
我们分析了颈动脉狭窄实验合作(CSTC)数据库的四个随机对照试验中有症状的颈动脉狭窄患者的个体水平数据。只包含试验中病人随机分配到CAS或CEA组的且为症状性狭窄患者的研究。评估5年组人群周期性时间的(从随机到120天)卒中和死亡风险以及CAS或CEA组病人长期随访的同侧卒中风险。所有分析都在意向性治疗基础上完成。
在这些随机对照试验中,对于年龄70 - 74岁及以上的患者,CAS明显优于CEA。CAS治疗组病人的周期性卒中风险增加完全是由于年龄的差异。年龄对CEA治疗组或任一治疗的周期性风险影响非常小。
原始出处:
George Howard, Prof Gary S Roubin, et al,Association between age and risk of stroke or death from carotid endarterectomy and carotid stenting: a meta-analysis of pooled patient data from four randomised trials,lancet,12 February 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#内膜#
46
#风险的关系#
49
#置入术#
47
#Lancet#
39
#死亡风险#
35
#切除术#
39