为何海拔较高地区肺癌发病率低
2015-01-20 王英 生物通
瑞士医生Paracelsus说:“所有物质都是毒物,非毒物是不存在的,仅仅是量的多少左右了它们毒性的大小。”根据PeerJ最近发表的一项最新研究表明,即使氧气也可能发生上面所描述的情况。虽然氧气在人类生活中不可或缺,但氧代谢的某些方面可能会促发癌症。利用氧浓度与海拔高度呈反比的关系,研究人员发现,在海拔较高的地区肺癌发病率较低,这一趋势没有延伸至非呼吸道肿瘤,从而表明致癌物质是通过吸入而发生的。
瑞士医生Paracelsus说:“所有物质都是毒物,非毒物是不存在的,仅仅是量的多少左右了它们毒性的大小。”根据PeerJ最近发表的一项最新研究表明,即使氧气也可能发生上面所描述的情况。虽然氧气在人类生活中不可或缺,但氧代谢的某些方面可能会促发癌症。利用氧浓度与海拔高度呈反比的关系,研究人员发现,在海拔较高的地区肺癌发病率较低,这一趋势没有延伸至非呼吸道肿瘤,从而表明致癌物质是通过吸入而发生的。
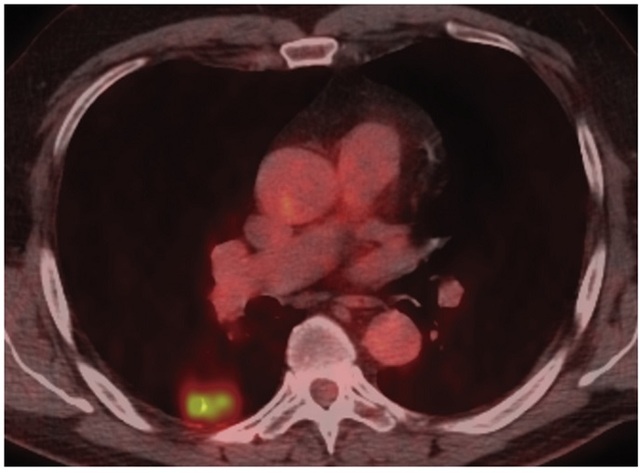
在美国,肺癌引起27%的癌症死亡,每年夺去160,000人的生命。虽然吸烟与高达90%的肺癌病例有关,但是这项新的研究表明,大气中的氧气可能在肺癌的发生发展过程中发挥作用。
氧气是高反应性的,即使在它在被我们细胞仔细和快速消耗的时候,它会引起活性氧物种(ROS)——可导致细胞损伤和突变。然而氧气组成整个大气的21%,海拔较高地区的低压会引起较少的吸入氧——这一影响众所周知会挫败高海拔地区的运动员。例如,在美国一些县之间,海拔差异可导致从加州因皮里尔县(-11 m)科罗拉多圣胡安县(3473 m)的氧水平减少34.9%。
为了探讨吸入氧是否可能是一种人类致癌物,宾夕法尼亚大学和加州大学的两名研究人员,比较了美国西部不同海拔县市之间的癌症发生率。他们发现,随着这些县市海拔高度的增加,肺癌的发病率逐渐降低。这种效果非常明显,海拔每上升1000米(3281英尺),每100,000人当中就减少7.23例病例,相当于平均大约13%的肺癌发病率。各种统计技术证明这种关联性并非偶然。
所观察到的关联性并不能证明氧气会导致肺癌。这项研究关注的是群体而不是个人,除了氧水平之外,还有许多变量与海拔有关。因此,研究人员进行了深入分析,以探讨潜在的混淆因素。他们的模型对重要风险和人口变量做出了解释,例如吸烟率和教育程度。这一关联在群体亚组、州和模型之间是一致的。
研究人员还评估了乳腺癌、结肠癌和前列腺癌:美国其余三大最常见癌症。海拔与这些非呼吸道癌症之间的关联性很弱或者没有,从而支持吸入性风险因素的假设。此外,海拔相关的环境因素,例如日晒和细颗粒物(污染的一个衡量),与海拔本身相比,会产生非常差的肺癌发病率预测。
过去两项流行病报告——将海拔作为一个混杂因素,提出海拔依赖性氧变化是高海拔地区较低癌症死亡率的原因。不同于之前这两项研究,当前这项研究特别注重评估海拔的影响,并得益于最近越来越多的高质量县级数据。总的来说,这项研究依赖于超过30个变量,有足够的覆盖率和精确度,能够包括约250个美国西部县。利用高分辨率的人口普查数据,研究人员计算出可反映每个县内人口分散的海拔值,从而更准确地估算每个县人口的大气暴露。所有的资源是公用的,从而强调了开放数据对于未来科学发现的重要性。
作者希望有更多的研究人员将他们的注意力集中在“氧气在人类致癌作用中所扮演的角色”。对不同地区和个人层次数据集的分析,将带来进一步的流行病学证据。最终,完全控制的、实验性的、利用癌变模型的研究,将是理解这一现象的关键所在。
如果未来的分析确定氧气可驱动肿瘤发生,那么其医学意义是非常大的。但是,基于这一发现,作者并不推荐个人进行迁徙,但是确定一个通用的主要危险因素,可能会为肺癌的病因提供新的见解。根据这些见解,可能会产生更好的治疗和预防措施。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#癌发病#
24
#发病率#
29
#海拔#
33
氧毒性?还是与ROS有关?
103
#癌发病率#
31