JTO:Alectinib能用于ALK阳性的耐药的非小细胞肺癌脑转移治疗
2015-02-01 MedSci译 MedSci原创
Crizotinib和 Ceritinib是两种重要的ALK抑制剂,主要用于ALK阳性的非小细胞肺癌(NSCLC),然而,也面临患者快速耐药问题。以往研究表明Ceritinib对Crizotinib耐药的ALK阳性的NSCLC患者。那么,患者也对Ceritinib耐药,该如何处理呢?下一代ALK抑制剂Alectinib可能能解决这个问题。本研究发表在JTO上,主要用于ALK重排阳性的NSCLC患者
Crizotinib和 Ceritinib是两种重要的ALK抑制剂,主要用于ALK阳性的非小细胞肺癌(NSCLC),然而,也面临患者快速耐药问题。以往研究表明Ceritinib对Crizotinib耐药的ALK阳性的NSCLC患者。那么,患者也对Ceritinib耐药,该如何处理呢?下一代ALK抑制剂Alectinib可能能解决这个问题。
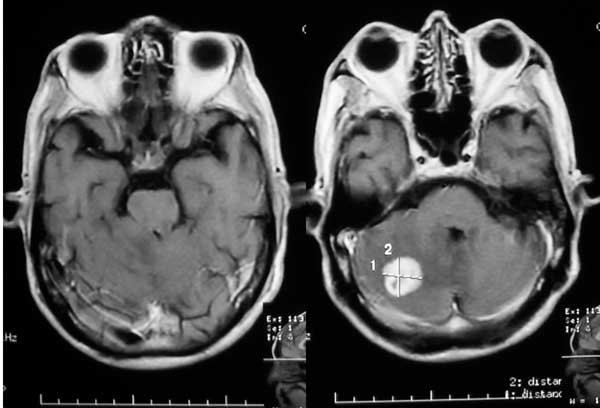
本研究发表在JTO上,主要用于ALK重排阳性的NSCLC患者脑转移,而且已对Crizotinib和 Ceritinib是两种重要的ALK抑制剂耐药的患者。采用alectinib 600 mg一天两次,共治疗4例患者。
结果发现,4名ALK阳性且有脑膜转移的患者,其中3例获得良好的效果,而且在放射学表现上看,效果很明显。第4位患者脑内病灶稳定达到4个月。而且总体来说,患者耐受良好,只有一例患者有2级高胆红素血症。
这个研究结果初步显示alectinib 对耐药的且有脑转移的ALK患者显示出良好的前景。
原始出处:
Gainor JF, Sherman CA, Willoughby K, Logan J, Kennedy E, Brastianos PK, Chi AS, Shaw AT.Alectinib Salvages CNS Relapses in ALK-Positive Lung Cancer Patients Previously Treated with Crizotinib and Ceritinib.J Thorac Oncol. 2015 Feb;10(2):232-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#非小细胞#
44
#Alectinib#
45
#ALK阳性#
35
好文章,攒
109
#转移治疗#
42
一代比一代强
135