Lancet Oncol:雷莫芦单抗+吉西他滨作为二线疗法可显著延长恶性胸膜间皮瘤患者的生存期!
2021-09-07 Nebula MedSci原创
雷莫芦单抗联合吉西他滨可显著延长一线治疗失败后的恶性胸膜间皮瘤患者的生存期!
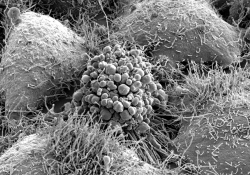
恶性胸膜间皮瘤是一种罕见的肿瘤,全球发病率不断增加,预后较差,5 年存活率不超过 10%。很少有患者适合接受包括根治性手术在内的多模式治疗,大多数患者仅接受抗癌药物治疗。自 2004 年以来,铂类和培美曲塞化疗一直是不可切除恶性的胸膜间皮瘤的标准治疗方法。
RAMES 研究是一项多中心、随机化、双盲的、安慰剂为对照的 2 期试验,旨在评估抗 VEGFR-2 抗体雷莫芦单抗联合吉西他滨治疗预处理过的恶性胸膜间皮瘤患者的疗效和安全性。
该研究在意大利的 26 家医院开展,招募了年满 18 岁的、ECOG 表现状态 0-2 分、组织学确诊的、在铂类+培美曲塞一线治疗期间或治疗之后进展的恶性胸膜间皮瘤患者。受试患者被随机(1:1)分至两组,接受吉西他滨(1000 mg/m2,第1和8天/3周)联合雷莫芦单抗(10 mg/kg,第1天/3周)或安慰剂治疗,直到病情进展或出现不可耐受的毒性。主要终点是总生存期。
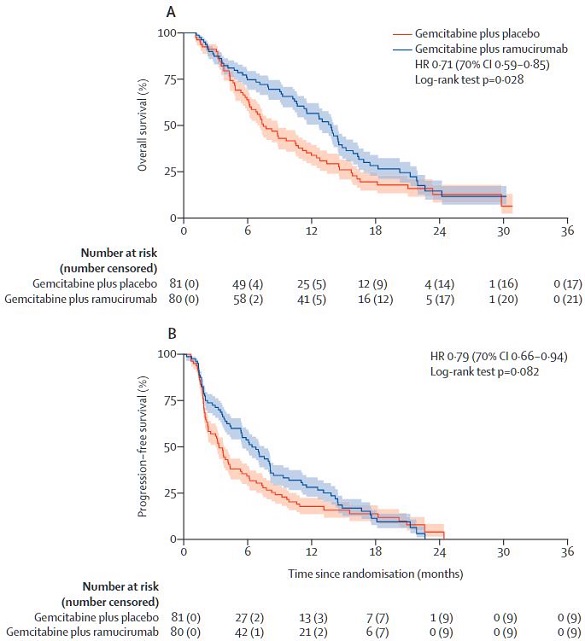
两组患者的总生存期和无进展生存期
2016年12月22日至2018年7月30日,共 161 位患者接受了吉西他滨+安慰剂(n=81)或吉西他滨+雷莫芦单抗(n=80)治疗。截止2020年3月8日,中位随访了 21.9 个月(范围 17.7-28.5 个月)后,雷莫芦单抗组的总生存期长于安慰剂组,中位总生存期分别是 13.8 个月和 7.5 个月(HR 0.71, 70%CI 0.59-0.85; p=0.028)。雷莫芦单抗和安慰剂组的中位无进展生存期分别是 6.4 个月和 3.3 个月(p=0.082)。
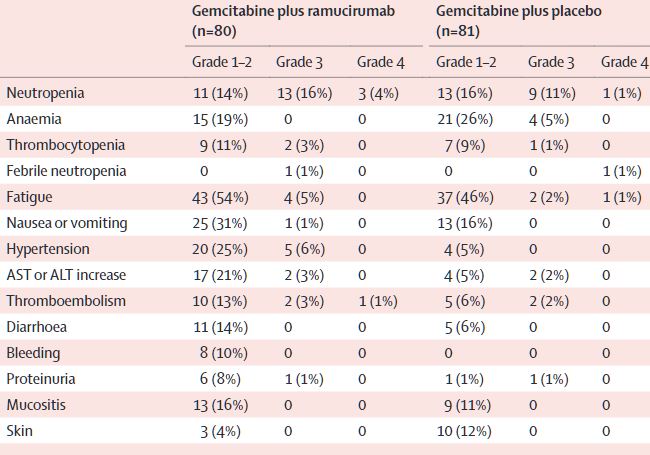
不良事件发生情况
雷莫芦单抗组和安慰剂组分别有 35 位(44%)和 24 位(30%)患者报告发生了3-4 级治疗相关的不良事件。最常见的治疗相关的 2-4 级不良事件是中性粒细胞减少(雷莫芦单抗 vs 安慰剂组:20% vs 12%)。雷莫芦单抗和安慰剂组还分别有 5 位(6%)和 4 位(5%)患者报告了治疗相关的严重不良事件,最常见的是血小板减少症(4% vs 2%)。无治疗相关死亡。
综上,对于采用标准化疗治疗后进展的恶性胸膜间皮瘤患者,雷莫芦单抗联合吉西他滨可较吉西他滨单药治疗显著延长其总生存期,而且安全性良好。该联合方案或可纳入这类患者的治疗选择。
原始出处:
Carmine Pinto, et al. Gemcitabine with or without ramucirumab as second-line treatment for malignant pleural mesothelioma (RAMES): a randomised, double-blind, placebo-controlled, phase 2 trial. The Lancet Oncology. September 06, 2021. https://doi.org/10.1016/S1470-2045(21)00404-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#雷莫芦单抗#+#吉西他滨#作为二线疗法可显著延长恶性#胸膜间皮瘤#患者的生存期
70
#Oncol#
31
#Lancet#
35
#胸膜#
46
#生存期#
27
#间皮瘤#
43
爱情雨绝了昆特吐鲁番市
55
顶刊就是不一样,质量很高,内容精彩!学到很多
56
谢谢梅斯分享这么多精彩信息
57
谢谢梅斯分享这么多精彩信息
0