骨巨细胞瘤术后复发 确定病变性质是关键
2017-09-22 牛晓辉 郝林 骨肿瘤
24岁男性患者,骨巨细胞瘤术后定期复查,复查X 线检查,发现右胫骨溶骨性病灶面积逐渐扩大,考虑骨巨细胞瘤复发。如何确定病变性质?主要治疗方法为手术切除——囊内切除和边缘切除又各有何特点?如何选择手术边界?
24岁男性患者,骨巨细胞瘤术后定期复查,复查X 线检查,发现右胫骨溶骨性病灶面积逐渐扩大,考虑骨巨细胞瘤复发。如何确定病变性质?主要治疗方法为手术切除——囊内切除和边缘切除又各有何特点?如何选择手术边界?
(1)病历介绍
:患者,男,24岁,主因左胫骨近端骨巨细胞瘤术后5个月,门诊收入院。患者于5个月前因左胫骨近端骨巨细胞瘤在当地医院行左胫骨上段骨巨细胞瘤刮除植骨术。术后病理为“骨巨细胞瘤”。术后定期复查,复查X 线检查,发现右胫骨溶骨性病灶面积逐渐扩大,考虑骨巨细胞瘤复发。为进一步诊治来我院,遂收入院。
入院查体:左膝关节后方可见长约10cm的陈旧性手术瘢痕。左膝关节无肿胀,皮肤颜色正常,无静脉曲张,皮温正常。左膝关节无压痛,屈伸活动无明显受限。左足背动脉搏动有力。
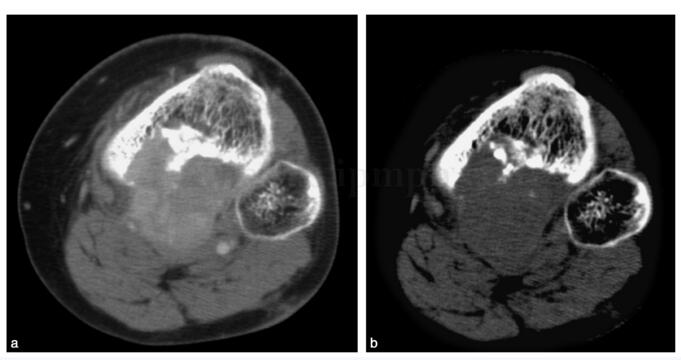
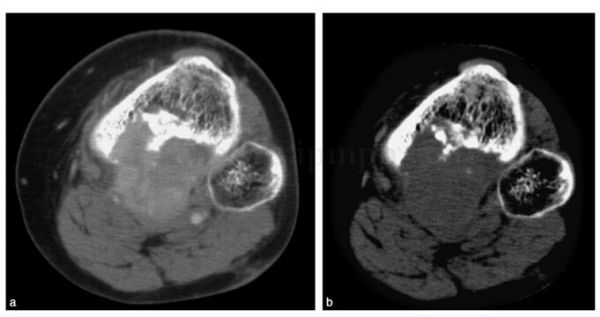
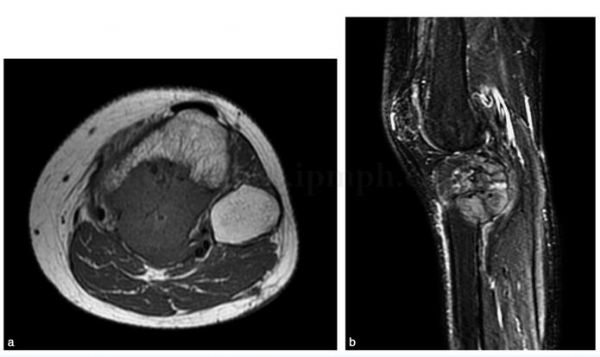
影像学检查:X 线示左胫骨上端可见高密度植骨影,植骨下方可见溶骨性破坏,根据患者连续复查X 线片表现,溶骨性破坏面积逐渐增大。病变边界清楚,骨皮质不连续,无骨膜反应,可见软组织包块(图6‐1)。左胫腓骨CT 显示为左胫骨上端溶骨性破坏,局部可见植骨。空腔密度均匀,边界清楚,可见骨皮质不连续,无骨膜反应,可见软组织包块。软组织包块可不均匀强化(图6‐2)。MRI 可见胫骨后侧异常信号,从胫骨向后突出。(图6‐3)
图6‐2 CT 胫骨后方破坏,有软组织包块
图6‐3 MRI 片
常规化验检查正常。
术前行病变穿刺活检,病理报告为送检组织中见较多量破骨细胞样多核巨细胞和卵圆形核的单核基质细胞,单核细胞异型性不明显,结合临床病史及影像学,诊断:骨巨细胞病变,首先考虑骨巨细胞瘤,鉴于患者肿瘤复发,皮质有破坏及软组织包块,待更多标本进一步分析有无分化差的区域。
完善术前准备后,在联合麻醉下行左胫骨近端瘤段截除,人工关节置换术。患者取平卧位,在止血带下操作。手术选择胫前内侧切口,梭形切除穿刺活检道,切开皮肤、皮下,切断附着于胫骨上段的胫前肌,鹅足,髌腱,关节囊,交叉韧带,去除腓骨小头,后侧肿瘤有肌覆盖,分离动静脉,将肌同肿瘤一并切除。距关节11cm切断胫骨,完整切除肿瘤。清除
窝处原手术瘢痕。彻底止血后安装假体,用MESH 包裹假体,重建髌腱,转移腓肠肌内侧头,覆盖假体,将髌腱缝合于假体与MESH 上,同时和外侧深筋膜和腓肠肌肌瓣加强。冲洗伤口,放引流管3 根,关闭伤口,加压包扎。长腿石膏后托制动。
术后常规应用抗生素,引流量<20ml 后拔除引流管。
术后两周拆线,制动8周后进行膝关节功能锻炼。定期复查。
(2)专家分析
:骨巨细胞瘤为良性侵袭性病变(Enneking 分期为3 期),可以复发和发生肺转移。好发年龄20~40岁,好发部位长骨骨端(股骨下端、胫骨上端、股骨上端、肱骨上端,桡骨远端等),此外椎体、骶骨也可见。主要症状为疼痛、肿胀,可有病理性骨折。化验检查无特殊。X 线检查典型特点为偏心、膨胀、溶骨。CT 有强化。
病理特点:大体标本为黄褐色质脆组织,合并动脉瘤样骨囊肿可见囊腔。镜下主要成分为多核巨细胞和基质细胞(梭形细胞),无成骨和钙化。
治疗:囊内切除或边缘切除。囊内切除有一定的复发率。单纯刮除植骨复发率可达20%以上,现在采取扩大刮除,复发率降到了12%以下。但刮除术要求病灶有比较好的骨壳,术中采用物理、化学方法,达到扩大的外科边界,以降低复发率。边缘切除,需要重建功能,往往都要损失许多功能,给患者造成一定的功能障碍。
(3)诊断要点
:该患者为骨巨细胞瘤术后复发病例,患者于5个月前在外院诊断为左胫骨近端骨巨细胞瘤,行病灶清除植骨术,病理证实为骨巨细胞瘤。术后定期门诊复查,X 线可见植骨部位溶骨性低密度病灶,病灶面积随时间推移逐渐增大。由于病灶刮除植骨之后存在植骨吸收问题,在诊断肿瘤复发及植骨吸收时可能存在困难。此时CT 检查有助于发现有无骨皮质破坏。该患者CT 检查可见骨皮质不连续,胫骨近端后方可见软组织包块,包块可不均匀强化。
骨巨细胞瘤复发患者需考虑肿瘤有无恶变及肺部转移情况发生。我们认为需行病变穿刺活检确定病变性质。穿刺活检时需考虑患者可能手术治疗方法及手术入路。穿刺部位必须位于手术入路上,以便手术时切除活检针道。该患者拟胫骨前内侧入路,故穿刺部位选择在胫骨内侧。该患者穿刺活检病理报告为骨巨细胞病变,首先考虑骨巨细胞瘤。患者肺CT检查未发现明显转移病灶。结合患者病史、临床表现、影像学检查及穿刺活检病理结果,骨巨细胞瘤复发的诊断成立。
(4)治疗原则
:骨巨细胞瘤为良性侵袭性病变(Enneking 分期为3 期)。主要治疗方法为手术切除,手术可采用囊内切除或边缘切除。囊内切除有一定的复发率。单纯刮除植骨复发率可达20%以上,现在采取扩大刮除,复发率降到了12%以下。但刮除术要求病灶有比较好的骨壳,术中采用物理、化学方法,达到扩大的外科边界,以降低复发率。边缘切除,需要重建功能,往往都要损失许多功能,给患者造成一定的功能障碍。所以手术边界的选择,必须要在术前评估(影像学和病理),以选择恰当的外科边界。
(5)随诊结果
:患者术后未见明显并发症,术后4周开始股四头肌锻炼,术后8周开始练习膝关节屈伸活动,术后3个月时膝关节可伸至0°,屈至80°(图6‐4)。
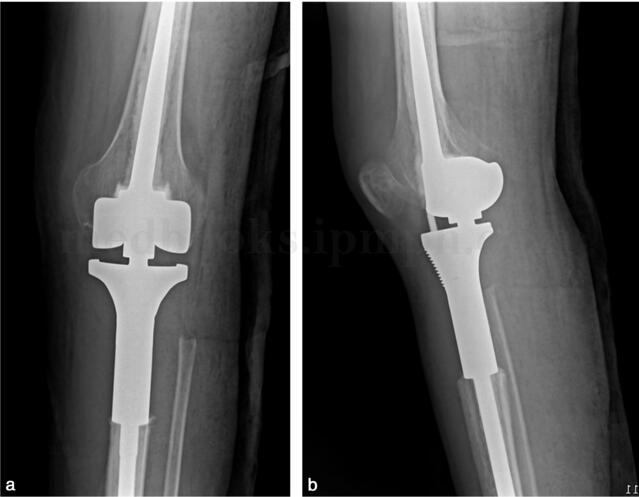
图6‐4 人工假体置换

图6‐5 正后方切口应尽量避免
现每3个月复查1次,无肺转移,局部无复发。
(6)经验教训
:患者第1次采用刮除植骨术,选的是膝关节后方切口(图6‐5),由于后侧有动静脉和坐骨神经,影响手术视野,术中操作不便。同时给二次手术带来很大问题,由于人工关节无法采用后方入路,所以二次手术采用的是前方入路,不能切除手术瘢痕,有一定的复发隐患。所以手术入路的选择,是手术设计上很重要的一步,有时直接影响手术的成败。
我们采取边缘切除,而不是囊内刮除。主要考虑到复发病例,虽然穿刺病理无恶变,但细胞生长活跃;其次,后侧有软组织包块,刮除时后侧充分显露比较困难,不易做到扩大的外科边界。
胫骨人工假体主要的问题是伸膝装置重建和假体前方覆盖。我们采取的方法是在假体上包裹生物补片(MESH),将髌韧带先和补片缝合,再和胫前深筋膜加强。Ⅰ期转移腓肠肌肌瓣,覆盖假体前方,术后膝关节制动于伸直位8周,功能锻炼。
复发病例,复查时要做肺部CT,警惕肺转移。
参考文献
1.Campanacci M,Baladini N,Boriani S,et al.Giant cel tumor of bone.J Bone Joint Surg,1987,69:106‐114
2.O’Donnel R J,Springfield D,S.Motwani HK,et al.Recurrence of giant‐cel tumors of the long bones after cu ret age and packing with cement.J Bone Joint Surg,1994,76:1827‐1833
3.Malawer MM,Bickels J,Mel er J.Cryosurgery in the treatment of giant cel tumor a long‐term fol ow‐up study. Clin Orthop,1999,359:176‐188
4.Ward WG,Li G.Customized treatment algorithm for giant cel tumor of bone.Clin Orthop,2002,397:259‐270
5.Bini SA,Gil K,Johnston JO.Giant cel tumor of bone.Clin Orthop,1995,321:245‐250
6.Sung HK,Kuo DP,Shu WP,et al.Giant cel tumor of bone:Analysis of two hundred and eight cases in Chinese patients.J Bone Joint Surg,1982,64:755‐761
7.Cheng CY,Shih HN,Hsu KY.Treatment of giant cel tumor of the distal radius.Clin Orthop,2001,383:221‐228
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#术后复发#
34
#病变性质#
38
#变性#
32
#细胞瘤#
26
#骨巨细胞瘤#
41
#巨细胞#
30