J Clin Periodontol:牙周病患者牙周支持治疗期间的口腔健康相关生活质量如何?
2021-12-09 MedSci原创 MedSci原创
牙周病(PD)的发病率很高,据估计,重度牙周炎影响了全球5.38亿人(发病率为7.4%)。如果不进行治疗,PD会出现牙龈肿胀和出血、牙齿移位等症状,并最终导致牙齿脱落。
牙周病(PD)的发病率很高,据估计,重度牙周炎影响了全球5.38亿人(发病率为7.4%)。如果不进行治疗,PD会出现牙龈肿胀和出血、牙齿移位等症状,并最终导致牙齿脱落。此外,无论PD严重程度如何,都会降低患者口腔健康相关生活质量(OHRQoL)。近日,一项为期两年的随机对照试验中,研究人员评估了牙周支持治疗(SPT),包括仅有口腔卫生指导的口腔预防(试验组) VS. 龈下器械治疗相结合(对照组),对口腔健康影响档案(OHIP-14)的影响。

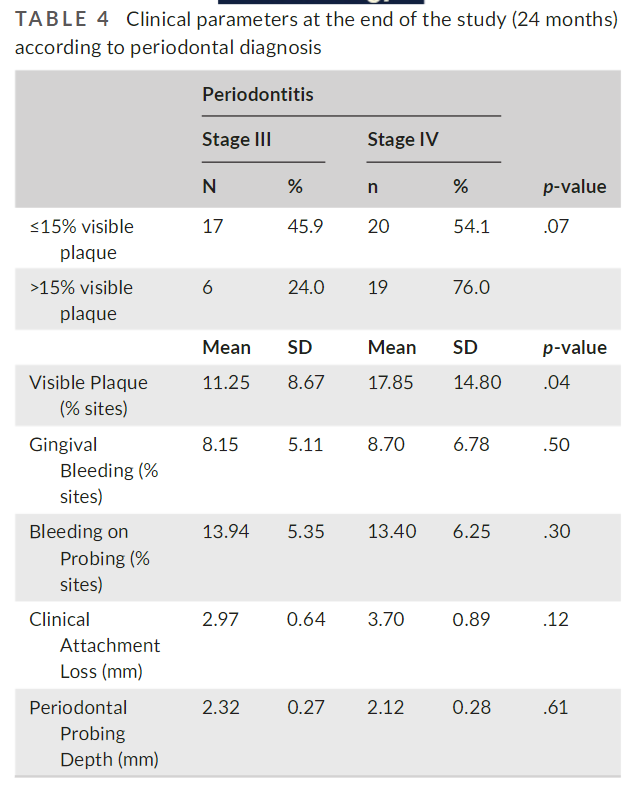
研究在基线、6、12、18和24个月时评估OHIP-14。通过GEE和Logistic回归分析了62名参与者(50.97±9.26岁,24名吸烟者)的数据。计算了OHIP-14的平均值、效应大小、最低和最高效应以及最小重要差异。计算了OHIP-14的总和(严重程度)、"相当经常"(FO)或 "非常经常"(VO)的反应数(程度)以及报告FO或VO的人的百分比(流行率)。
结果显示,在基线时,试验组(7.67±9.27)和对照组(6.51±7.47)的OHIP-14得分较低,在SPT期间呈下降趋势,组间或组内随时间推移没有差异。在6个月时,观察到OHIP-14的患病率有差异(p = .03),在PD严重程度和范围上没有差异。在24个月时,吸烟状况和菌斑>15%(口腔卫生中度)与该时间点较高的OHIP-14流行率值有关(分别为p=0.038和p=0.034)。
综上所述,该研究结果表明,接受两种不同模式的SPT治疗的患者在2年的护理中保持较低的OHIP-14得分。
原始出处:
Marina Mendez, et al., Oral health-related quality of life during supportive periodontal therapy: results from a randomized clinical trial. J Clin Periodontol. 2021 Aug;48(8):1103-1110. doi: 10.1111/jcpe.13473.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#支持治疗#
0
#PE#
34
#牙周病#
57
#牙周#
53
#健康相关生活质量#
42