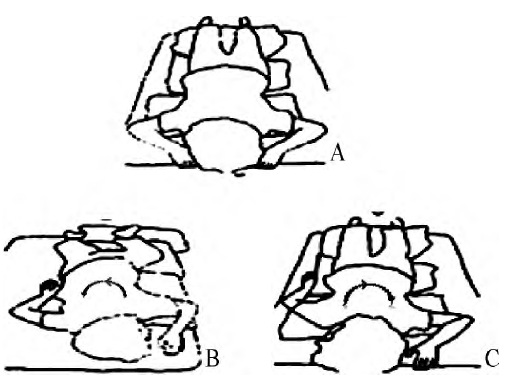
俯卧位手术全麻苏醒期加强型气管导管部分断裂一例
2019-10-22 张晓宇 段宗生 孙艳平 临床麻醉学杂志
患者,男,58岁,因腰椎间盘突出症于全麻下行腰椎后路椎间盘髓核常规摘除术。既往体健,无酗酒史。麻醉诱导顺利,予喉镜明视下置入ID7.5mm加强型气管导管,导管深度22 cm,使用胶布固定,行机械通气,静-吸联合麻醉维持。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#苏醒#
42
#部分断裂#
42
#气管导管#
43
#俯卧位#
29
#全麻#
47