Nat Genet:GWAS分析发现增加子宫内膜癌风险的新变异
2016-05-05 生物谷 生物谷
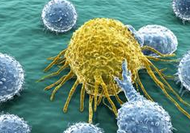
2016年5月5日讯 /生物谷BIOON/ --最近一项国际合作发现了可能增加女性患子宫内膜癌风险的五个新基因区域,子宫内膜癌是影响女性的一种常见癌症类型,该研究将与该疾病有关的已知基因区域增加到九个。 子宫内膜癌是发生在子宫壁的癌症,在英国每年有大约9000人新诊断为该疾病。来自剑桥大学,牛津大学等研究单位的研究人员对超过7000名患病女性和大约37000名健康女性的DN

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Genet#
33
#NET#
41
#Nat#
30
#新变异#
33
#内膜#
41
#Gene#
30
#癌风险#
37
现在全基因组的都能大三杂志
147
不错啊!
131
测序就能发文章
94