Pediatr Rheumatol Online J:牙周炎或是CCP抗体阳性的幼年特发性关节炎的一个发病因素
2016-02-21 MedSci MedSci原创
Pediatr Rheumatol Online J:牙周炎或是CCP抗体阳性的幼年特发性关节炎的一个发病因素已知类风湿性关节炎与牙周炎之间具有关联。一些患有幼年特发性关节炎(JIA)的儿童其表型与成人类风湿性关节炎相似,其特点是存在抗环瓜氨酸肽(CCP)抗体。本研究试图探讨CCP阳性的JIA与牙周炎的症状以及口腔微生物的抗体之间的关系。研究共纳入71名CCP阳性的JIA的儿童和74名CCP阴性的
目标
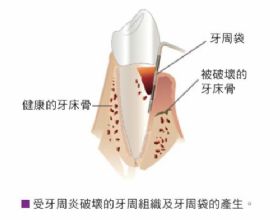
已知类风湿性关节炎与牙周炎之间具有关联。一些患有幼年特发性关节炎(JIA)的儿童其表型与成人类风湿性关节炎相似,其特点是存在抗环瓜氨酸肽(CCP)抗体。本研究试图探讨CCP阳性的JIA与牙周炎的症状以及口腔微生物抗体之间的关系。
方法
研究共纳入71名CCP阳性的JIA儿童和74名CCP阴性的JIA儿童,使用ELISA法检测其口腔病原菌牙龈卟啉单胞菌、中间普氏菌以及具核梭杆菌的抗体。共收集了37名CCP阳性和121名CCP阴性的JIA的儿童的口腔健康病史。采用t检验、卡方检验、Mann–Whitney U检验以及多元回归对比两组的数据。
结果
结果发现,与CCP阴性的JIA儿童相比,CCP阳性的JIA儿童更可能是女性,年龄稍大一些以及非白种人群。CCP阳性的儿童其抗牙龈.卟啉单胞菌和中间普氏菌的IgG抗体效价较高,校正年龄后,牙龈卟啉单胞菌的抗体效价仍明显高于CCP阴性的儿童,差异具有统计学意义。与CCP阳性的JIA的儿童相比,与CCP阴性的JIA的儿童更容易出现牙龈出血(24% VS. 43%)。纳入研究对象时匹配了年龄,CCP阳性的JIA儿童牙龈出血的几率或倾向较CCP阴性的JIA儿童高2.2倍。
结论
总而言之,本研究发现与CCP阴性的JIA儿童相比, CCP阳性的JIA儿童牙龈卟啉单胞菌的抗体滴度较高,口腔健康不佳的症状更多,表明牙周炎或在CCP阳性的JIA病因中发挥了一定的作用。
原始出处:
Lauren Lange, Geoffrey M. Thiele, et al. Symptoms of periodontitis and antibody responses to Porphyromonas gingivalis in juvenile idiopathic arthritis. Pediatr Rheumatol Online J. 2016; 14: 8. Published online 2016 Feb 9. doi: 10.1186/s12969-016-0068-6.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#抗体阳性#
34
#DIA#
32
#特发性#
37
#PE#
46
好文章,还会关注
62
赞一个!拜读了并认真学习了。
63
#关节炎#
26
#牙周#
28