NEJM:哌唑嗪对退伍军人创伤后应激障碍的疗效分析!
2018-02-08 xing.T MedSci原创
由此可见,在这个涉及有慢性PTSD的退伍军人试验中,哌唑嗪并没有减轻恶梦的发生或改善睡眠质量。
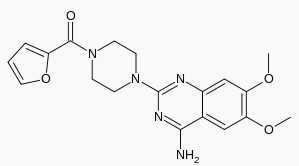
近日,顶级医学期刊NEJM上发表了一篇研究文章,在这项随机试验中,研究人员旨在证实哌唑嗪(一种α1-肾上腺素受体拮抗剂)可以有效地缓解了退伍军人创伤后应激障碍(PTSD)相关的噩梦。
研究人员从13个退伍军人事务部医疗中心招募了退伍军人,这些退伍军人患有慢性PTSD,并自我报告经常做恶梦。参与者被随机分配接受哌唑嗪或安慰剂治疗26周;药物或安慰剂在5周的过程中以分次递增的剂量给药,每天男性最多20mg和女性12mg。在第10周后,参与者继续以双盲方式再接受哌唑嗪或安慰剂额外治疗16周。三个主要结局指标是从基线到10周的临床医生给予的PTSD量表(CAPS)项目B2(“经常性恶梦”,得分范围从0到8,分数越高表示越频繁和梦境更痛苦)得分变化; 基线到10周的匹兹堡睡眠质量指数(PSQI;得分范围从0到21,分数越高表示睡眠质量越差)得分变化;以及治疗10周时的临床整体印象变化(CGIC)评分(评分范围从1到7,分数越低表示改善越大,评分为4表示没有改变)。
该研究总共纳入了304名参与者进行随机分组; 152人被分配到哌唑嗪组,152人被分配到安慰剂组。在10周时,哌唑嗪组与安慰剂组在CAPS项目B2评分(组间差异为0.2; 95%可信区间[CI]为-0.3至0.8,P=0.38)、PSQI评分(组间差异为0.1,95%CI为-0.9至1.1,P=0.80)和CGIC评分(组间差异为0,95%CI为-0.3至0.3; P=0.96)的平均变化没有显著差异。这些指标在26周(次要结局)或其他次要结果中没有显著差异。在10周时,平卧位收缩压与基线相比,哌唑嗪组和安慰剂组之间的平均差减少了6.7 mmHg。新发生的或恶化的自杀意念不良事件在被分配到哌唑嗪组的参与者中为8%,而在分配到安慰剂组的参与者中为15%。
由此可见,在这个涉及有慢性PTSD的退伍军人试验中,哌唑嗪并没有减轻恶梦的发生或改善睡眠质量。
原始出处:
Murray A. Raskind,et al. Trial of Prazosin for Post-Traumatic Stress Disorder in Military Veterans.NEJM.2018. http://www.nejm.org/doi/full/10.1056/NEJMoa1706640?query=featured_home
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#哌唑嗪#
36
#退伍军人#
43
#疗效分析#
36
#创伤#
38
#应激#
41
学习了新知识
75
学习了新知识
64
学习了新知识
64
学习了新知识
87
学习了新知识
69