鉴别诊断:T1高信号肝脏病变
Differential Diagnosis:T1 Bright Liver Lesions
①
T1高信号并黑环,T1高信号并黑环,无强化
-
T1 bright with a dark rim
-
T2 bright with a dark rim
-
No enhancement
-
No enhancement
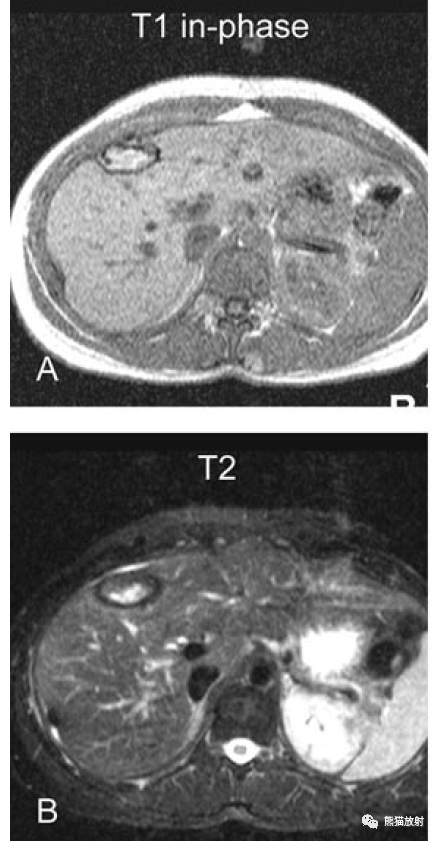
术后血肿
Hematoma after surgery
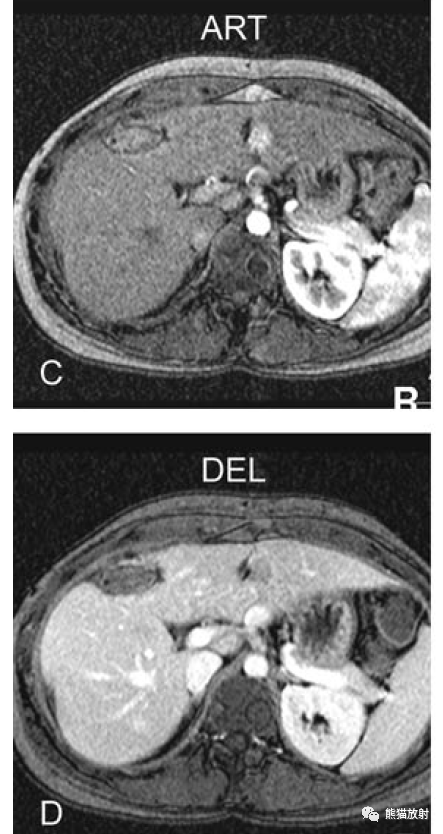
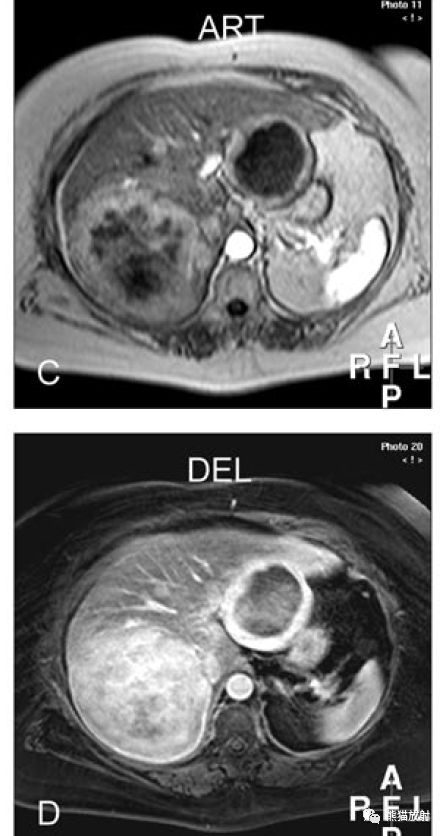
②
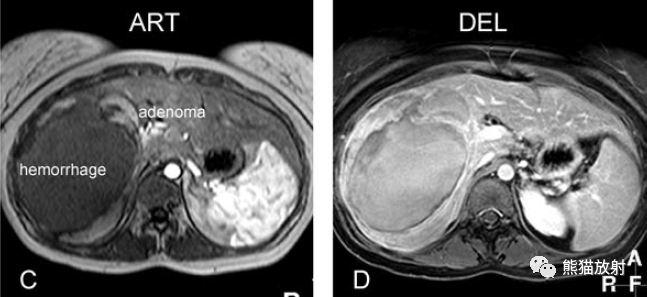
T1高信号并低信号病灶,T2低信号并好信号病灶,病灶不均质强化,实性部分有廓清
-
T1 very bright within a dark lesion
-
T2 dark with a bright lesion
-
Heterogeneous enhancement within the lesion
-
Washout within the solid lesion
类癌肝转移瘤并出血
Hemorrhagic carcinoid metastasis
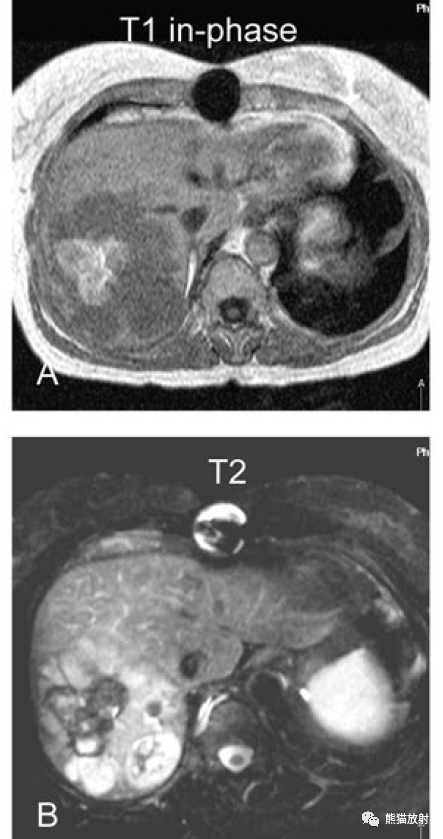
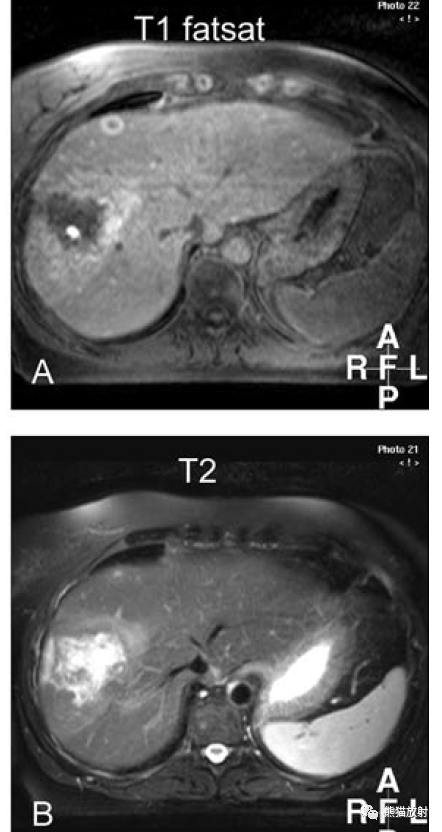
③
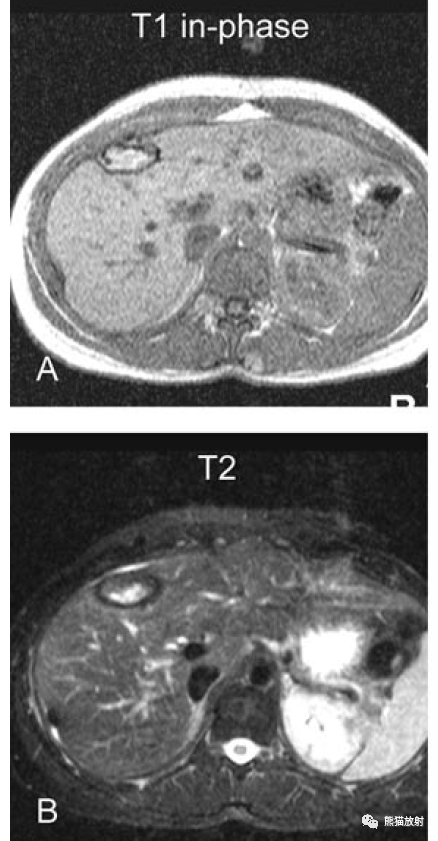
T1高信号并低信号病灶,T2混杂信号,不规则环形强化,不均质、持续强化
-
T1 bright and dark lesions
-
T2 mixed signal intensity
-
Irregular ring-shaped enhancement
-
Heterogeneous and persistent enhancement

类癌肝转移瘤并蛋白产生
Protein-producing carcinoid metastasis
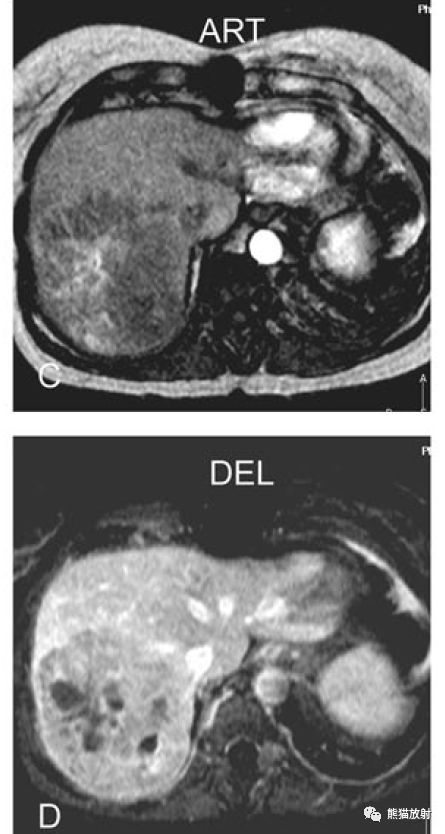
④
T1主要为高信号,T2等至明亮高信号,T1高信号部分有强化,不均质持续强化
-
T1 (predominantly) bright lesions
-
T2 isointense to very bright
-
Enhancement of the T1-bright parts
-
Heterogeneous and persistent enhancement
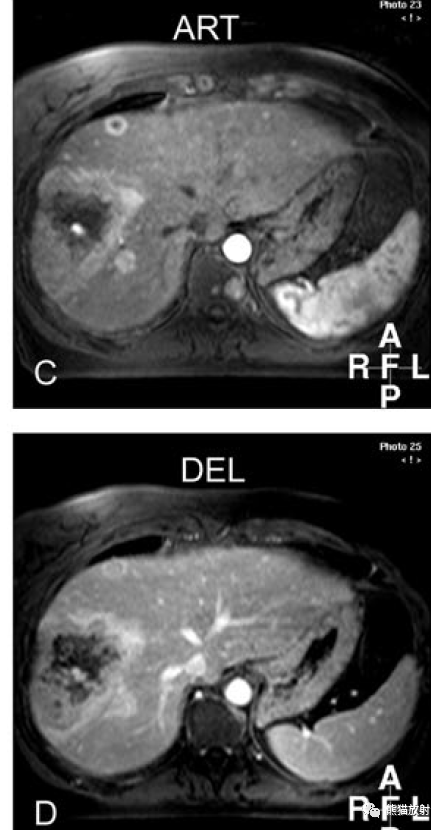
黑色素瘤肝转移
Melanoma metastases
小结
-
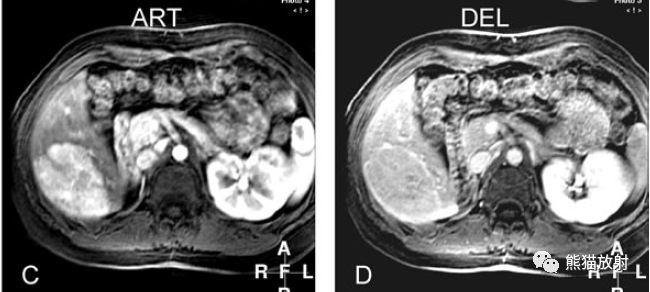
评估T1WI:所有病变在非肝硬化肝脏内都有高信号的成分。在第一个病例中,病变被黑色的边缘包围。第二个病例可见中心明亮高信号区域。第三例显示左肝内囊性病变并高信号内容物。第四例显示多个高信号病变并环状表现。
-
评估T2WI:第一例中,病变被厚度增加的低信号边缘包围。第二例显示较大病灶中心低信号。第三例显示两个高信号病灶,包括囊性和实性成分。第四例显示多发大小不等高信号病变。
-
评估增强动脉期:第一例病变没有任何强化,第二例可见不均匀强化,第三例和第四例病灶周边实性部分较厚,有强化。
-
评估增强延迟期:第一例病灶无强化,第二例表现为有廓清,伴有持续的不均匀强化,第三例、第四例病灶边缘持续不均质强化。
-
血肿:T1高信号是由于正铁血红蛋白,另可见边缘的含铁血黄素环;
-
出血性类癌转移、产生蛋白质的类癌转移:提示转移;无特异性表现;结合临床。
-
黑色素瘤转移:结合病史,T1高信号;典型的动脉期明显强化。
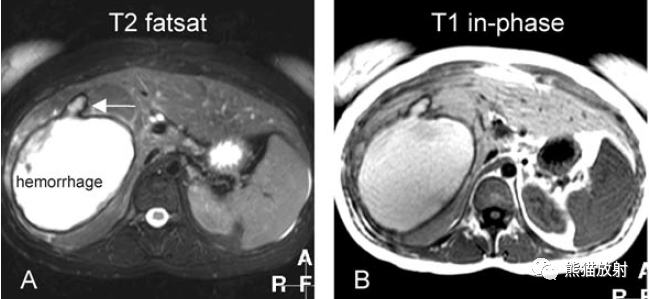
此外,肝细胞腺瘤易合并出血,同样可表现为T1高信号,边界清晰,动脉期明显强化,延迟期呈等信号,并见周围假包膜。合并大量出血时残留实性部分有强化。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#高信号#
41
#鉴别诊断#
53
受益匪浅
61