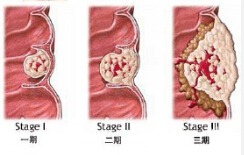
Lancet:贝伐与卡培他滨两药联用维持治疗结直肠癌使总生存期获益
2015-04-10 赵洲译 MedSci原创
新型药物的使用使得转移性结直肠癌的预后得到了改善。贝伐单抗是一种VEGF单克隆抗体,用于化疗可以出现显著的好处或者无进展存活期的存活率。因此,贝伐单抗被视为是一种标准的转移性结直肠癌的一线治疗选择。联合使用贝伐单抗对转移性结直肠癌患者进行化疗的最佳持续时间尚不明确。研究人员进行了卡培他滨结合贝伐单抗对转移性结直肠癌患者的维持治疗的有效性进行评估。 研究人员在荷兰的64所医院进行了此次非盲、临
新型药物的使用使得转移性结直肠癌的预后得到了改善。贝伐单抗是一种VEGF单克隆抗体,用于化疗可以出现显著的好处或者无进展存活期的存活率。因此,贝伐单抗被视为是一种标准的转移性结直肠癌的一线治疗选择。联合使用贝伐单抗对转移性结直肠癌患者进行化疗的最佳持续时间尚不明确。研究人员进行了卡培他滨结合贝伐单抗对转移性结直肠癌患者的维持治疗的有效性进行评估。
研究人员在荷兰的64所医院进行了此次非盲、临床三期的随机对照试验。受试者均是年龄超过18岁的成年人,之前已经患有未经治疗的转移性结直肠癌,病情稳定或者在六轮三周疗程的卡培他滨、奥沙利铂和贝伐单抗(CAPOX-B)治疗后病情改善。病人被随机均分为两组。病人和研究人员都知道治疗的具体分组情况。每九周对疾病状态进行评估。维持治疗包括每日两次口服卡培他滨625mg/m2加上贝伐单抗静脉注射(7.5mg/kg每三周一次)。
试验共有558名病人参与。279人分在了维持治疗组,另一半在观察组。平均跟踪随访48个月。主要监测指标是无进展存活率。试验表明,维持治疗可以很好地被接受。维持治疗导致了平均总存活时间出现了3.5个月的绝对增长。此次试验表明,卡培他滨联用贝伐单抗可以成为首选的治疗策略用于治疗非转移性结直肠癌。
原始出处:
Lieke H J Simkens et al.Maintenance treatment with capecitabine and bevacizumab in metastatic colorectal cancer (CAIRO3): a phase 3 randomised controlled trial of the Dutch Colorectal Cancer Group.Lancet.Published Online April 8, 2015 http://dx.doi.org/10.1016/S0140-6736(14)62004-3本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
22
#卡培他滨#
25
#生存期#
22
#结直肠#
31
#贝伐#
25
#总生存期#
22
不错的课程
74