Stroke:证实脑微血管损伤与脑血管周围间隙扩大有关
2016-04-01 MedSci MedSci原创
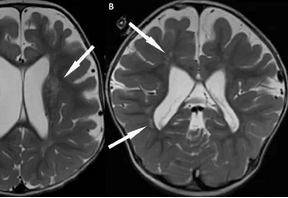
脑血管周围间隙扩大是公认的脑微血管损伤的影像学标记,但这两者之间的关系还未通过直接可视化的小血管来证实。我们调查了视网膜成像的微血管口径和大脑MRI血管周围间隙扩大(ePVSs)的关系。
脑血管周围间隙扩大是公认的脑微血管损伤的影像学标记,但这两者之间的关系还未通过直接可视化的小血管来证实。我们调查了视网膜成像的微血管口径和大脑MRI血管周围间隙扩大(ePVSs)的关系。
包含来自Rotterdam研究的704名受试者。通过半自动照相对视网膜眼底小动脉和小静脉进行测量。
在眼底视网膜小动脉和小静脉的管径测量半自动地照片。使用标准化的评级方法,计算半卵圆中心、基底神经节,海马体,中脑的ePVSs。使用负二项回归模型决定视网膜微血管口径与ePVSs的关系,校正年龄、性别、血管口径,大脑结构MRI标记和心血管危险因素。
结果发现,较窄的动脉和较宽的静脉口径与半卵圆中心和海马区域更多的ePVSs相关。半卵圆中心和海马体区动脉比值比(95%CI)是1.07 (1.01-1.14) 和1.13 (1.04-1.22),静脉分别是1.08 (1.01-1.16) 和1.09 (1.00-1.18)。这些联系独立于其他的脑MRI标志物和心血管风险因素。
结论:视网膜微血管口径与ePVSs相关,证实了微血管损伤与ePVSs相关的假说。
原市场处:
Mutlu U1, Adams HH1, Hofman A1, van der Lugt A1, et al,Retinal Microvascular Calibers Are Associated with Enlarged Perivascular Spaces in the Brain. Stroke. 2016 Mar 15. pii: STROKEAHA.115.012438. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#血管损伤#
37
#微血管#
34
#损伤#
39