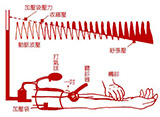
SC-ICC2015:孙宁玲--β受体阻滞剂可作为高血压一线治疗药物吗?
2015-04-15 佚名 心在线
2015年4月11日,在第17届中国南方国际心血管病学术会议“合理用药论坛”上,北京大学人民医院孙宁玲教授针对这一问题,以“β受体阻滞剂是否可以作为高血压治疗一线药物——国际指南引发β受体阻滞剂争议”为题,对这一重要问题做了详细诠释。关于β受体阻滞剂在高血压治疗中的地位问题,近些年一直存在较大争议,各国指南对其在高血压治疗中的应用给出了不同建议。指南对β受体阻滞剂的推荐有何不同?2004年英国NI
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#阻滞剂#
37
#受体阻滞剂#
37
#治疗药物#
39
#一线治疗药物#
42
该讲的详细些
133
还是有些糊涂,要是有详细机理更好
110
有道理
134
有道理
184
#β受体阻滞剂#
38
#ICC#
32