JAMA:颈动脉内膜中层厚度检测不能提高心血管事件风险评估效能
2012-11-26 MedSci JAMA
心血管疾病是全球范围患病率和致死率最高的疾病之一。对高风险无症状个体的预防性治疗则需基于准确的风险评价方法。目前无症状个体的风险预测主要靠心血管风险因素合并评分量表的分值水平。临床应用的数种评分量表中,Framingham风险评分是其中最广泛适用的。这些风险量表虽然表现不差,但在风险水平的评估中,部分心血管事件存在仍使评分存在一定误差。这就要求更好的心血管风险
心血管疾病是全球范围患病率和致死率最高的疾病之一。对高风险无症状个体的预防性治疗则需基于准确的风险评价方法。目前无症状个体的风险预测主要靠心血管风险因素合并评分量表的分值水平。临床应用的数种评分量表中,Framingham风险评分是其中最广泛适用的。这些风险量表虽然表现不差,但在风险水平的评估中,部分心血管事件存在仍使评分存在一定误差。这就要求更好的心血管风险预测工具,包括对亚临床动脉粥样硬化的测量。常规颈动脉内膜中层厚度(CIMT)检测能改善心血管事件绝对风险预测的评分效价的证据尚不一致。
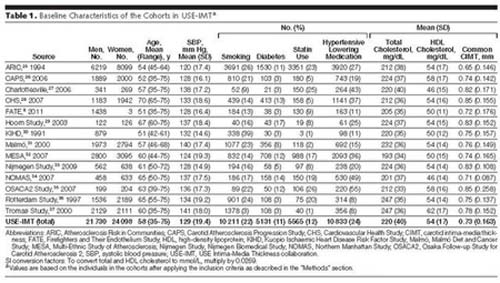
Den Ruijter博士等,就此问题进行一项meta分析,试图了解常规经动脉内膜中层厚度(CIMT)检测能否在使用Framinghan风险评分的基础上,改善对首次心肌梗死或卒中的10年内风险的预测价值。研究者通过检索PubMed1950年至2012年6月,及EMBASE1980年至2102年6月的相关研究和专家意见,捡取了以首次心肌梗死或卒中为随访终点、基线时常规行CIMT检查的普通人群研究。从上述研究中,将不存在心血管疾病的个体资料提取,建立数据库进行meta分析。
研究者从纳入的14个研究中,选取了共45828例研究对象的数据。在中位数为11年的随访期内,4007例发生首次心肌梗死或卒中。首先使用Framingham风险评分进行评估,随后加入常规CIMT测量结果,以评估10年发生首次心肌梗死或卒中的绝对风险。两种评估发生的C分析结果相似(0.757;95% CI,0.749-0.764;及0.759;95% CI, 0.752-0.766)。加入CIMT层顶后,再次分级改善率很小,仅为0.8%(95% CI, 0.1%-1.6%)。中危评价方面,所有研究对象的再次分级改善率为3.6%(95% CI, 2.7%-4.6%),性别之间无差异。
通过这个meta分析,研究者得出结果,在Framingham风险评估的基础上加做常规CIMT,对10年内新发心肌梗死或卒中的风险预测略有改善,但这一程度的改善并没有临床意义。
原始来源:
Den Ruijter HM, Peters SA, Anderson TJ, Britton AR, Dekker JM, Eijkemans MJ, Engström G, Evans GW, de Graaf J, Grobbee DE, Hedblad B, Hofman A, Holewijn S, Ikeda A, Kavousi M, Kitagawa K, Kitamura A, Koffijberg H, Lonn EM, Lorenz MW, Mathiesen EB, Nijpels G, Okazaki S, O'Leary DH, Polak JF, Price JF, Robertson C, Rembold CM, Rosvall M, Rundek T, Salonen JT, Sitzer M, Stehouwer CD, Witteman JC, Moons KG, Bots ML.Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA. 2012 Aug 22;308(8):796-803.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












收藏了!
129
#血管事件#
30
#内膜#
36
#颈动脉#
28
#心血管事件风险#
34
#颈动脉内膜中层厚度#
32