ACCF/AHA老年高血压专家共识解读
2011-07-29 MedSci原创 MedSci原创
高血压的预防重点一向集中在年轻人群,老年高血压相关预防研究十分缺乏。 4月25日,美国心脏病学会基金会与美国心脏学会联合发布《2011年老年高血压专家共识》。该共识是迄今为止国外首次专门针对老年高血压诊断、评估、管理和治疗发布专家共识,在全球人口老龄化的今天具有十分重要的意义。 2008年,我国首次发布了《中国老年高血压治疗专家共识》。近年来,老年高血压防治领域已取得不少进展,我国
高血压的预防重点一向集中在年轻人群,老年高血压相关预防研究十分缺乏。
4月25日,美国心脏病学会基金会与美国心脏学会联合发布《2011年老年高血压专家共识》。该共识是迄今为止国外首次专门针对老年高血压诊断、评估、管理和治疗发布专家共识,在全球人口老龄化的今天具有十分重要的意义。
2008年,我国首次发布了《中国老年高血压治疗专家共识》。近年来,老年高血压防治领域已取得不少进展,我国学者正着手对此版指南进行修订。美国《2011年老年高血压专家共识》的公布,无疑将为我国共识的修订提供重要参考价值。
老年高血压流行病学
1999~2004年间,美国18岁以上成人的高血压患病率为27%。高血压患病率随年龄增长而逐渐增加,弗雷明汉心脏研究显示,九成受试者在其55岁时血压尚正常,但最终均罹患高血压。
在美国老年人群中,高血压是最重要的心血管病危险因素,约69%的心肌梗死、77%的卒中和74%的心力衰竭(心衰)患者均有高血压病史。此外,高血压也是糖尿病、心房颤动和慢性肾病的主要危险因素。1995~2005年间,高血压致死率增加了25.2%,这一点在老年人群中尤为突出。
2009年美国直接或间接用于高血压防治的费用约为734亿美元。
老年高血压病理生理学
高血压发病率随年龄增长而明显增加,与增龄导致的动脉结构与功能改变有关。
增龄导致的大动脉硬化与动脉粥样硬化是截然不同的两个概念。后者在动脉硬化基础上发生,与其他心血管危险因素如糖、脂代谢异常等有关。而动脉硬化则由增龄所致,其机制尚不明确。
老年直立性低血压为人所关注。该共识指出,自主调节功能失常导致直立性低血压或直立性高血压。而事实上,在老年人群中,体位性血压改变所致血压升高亦较为常见。
导致老年人继发性高血压的因素较多。其中,肾动脉狭窄是常见的致病因素。尸检结果显示,肾动脉狭窄发病率为4%~50%,发病率随年龄增长而增加。
在65岁以上、无肾脏疾病和罹患外周动脉疾病的老年人群中,肾动脉狭窄>60%的超声检出率分别为6.8%和35%~50%。
其他与老年继发性高血压相关的因素包括阻塞性睡眠呼吸暂停、原发性醛固酮增多症、甲状腺功能亢进或低下、生活方式和药物等。
老年高血压患者终末器官损伤
该共识强调了高血压对老年患者心脏、肾脏、大动脉和外周血管的损害,并将高血压所致脑血管疾病和认知功能损害提升至十分重要的位置。老年高血压,尤其是单纯收缩期高血压(ISH)为脑缺血性卒中和脑出血的重要危险因素,并且卒中相关发病和死亡风险随年龄增长而增加。
在老年人群中,高血压患者的冠心病发病率明显高于血压正常者。此外,高血压也是心衰、左室肥厚、大动脉和外周动脉疾病的重要危险因素。 增龄和高血压均可导致肾功能损害,诱发慢性肾脏疾病,而后者又是老年人罹患冠心病和心衰的重要危险因素。
增龄和心血管危险因素的相互作用
各种心血管危险因素如冠心病早发家族史、血脂异常、糖尿病、肥胖、微量白蛋白尿、高同型半胱氨酸血症和高尿酸血症等,对老年高血压患者的影响明显大于年轻高血压患者。
由于各种危险因素的共同作用,加之增龄导致老年患者主要脏器功能衰退,使得老年高血压患者的心脑血管事件风险和并发症发生率明显高于年轻患者,相应处理也变得复杂,须合理治疗。
临床诊断与评估
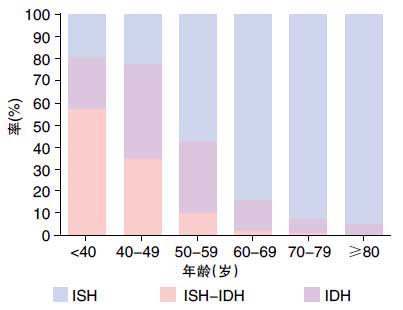
图不同年龄人群的未治高血压种类分布情况在老年高血压患者中,ISH较为多见,其发病率随年龄增长而增加。在60岁和70岁以上高血压人群中,ISH 患者比例为65%和逾
90%。IDH:单纯舒张期高血压。
老年高血压的临床评估内容包括病史询问、体格检查和诊断评估性实验室检查。该共识不推荐将既往高血压指南中提出的“常规实验室检查”,作为老年高血压评估的必要检查;建议对老年高血压患者行尿液(特别是尿蛋白/尿微量蛋白)、血生化(电解质、肾功能)、血脂、血糖(对糖尿病患者还须检查糖化血红蛋白)和心电图检查,对部分患者可行超声心动图检查。
老年人群的血压变异较大、影响因素较多,准确可靠的血压测量十分重要。高血压的诊断应以两个以上地点、3次不同时间的血压测量值作为依据。医生除外测量坐位血压,还应加测立位血压,并在初次对血压评估时,测量双臂血压,并随访观察测值较高一侧上肢的血压。
在体弱、服用各种降压或精神类药物的老年人群中,餐后低血压发病率较高。餐后血压测量可排除餐后低血压,这一点在我国专家中已达成共识。
假性高血压的准确识别在临床实践中十分重要,可避免老年人群过度降压,并减少不良事件发生。该共识指出,老年假性高血压的发病率为1.7%~70%,如此之大的发病率差异可能与不同研究的方法学有异有关,也与研究入组人群的不同特征有关。
有学者曾建议医生采用Osler手法鉴别假性高血压,但也有不同意见认为,Osler手法判断假性高血压的价值有限。至今仍无诊断假性高血压的简便、可靠方法,确诊有赖于有创性动脉内测压检查。
在医生评估老年人群的血压时,还应识别白大衣高血压。老年人群的白大衣高血压发生率高于年轻人,约为15%~25%。对于诊室血压升高、无靶器官损害的老年人群,动态血压监测可排除白大衣高血压。
此外,该共识还强调了踝部血压及诊室外血压测量(尤其是家庭自测血压),在老年高血压诊断评估中的重要性,值得借鉴。
血压管理推介
该共识推荐无并发症老年高血压患者的靶目标血压值为<140/90 mmHg,该目标血压值的确立来自专家建议、而非随机对照研究证据,目前尚不清楚这一血压值是否适用于80岁以上老年人群。
该共识强调了生活方式干预、生活质量、认知功能评估管理的重要性,尤其是对老年高血压患者的行为干预,应有别于年轻高血压患者。
该共识推荐的老年高血压预防仍以生活方式干预为主,如饮食控制、限盐、增加活动和减轻体重等。
在药物治疗方面,该共识肯定了药物治疗的益处,强调了老老年高血压患者降压研究(HYVET)的重要性,也指出了其不足。
老年高血压的药物治疗,应遵循小剂量起始用药、逐渐加量、充分考虑患者耐受性的原则。在血压控制不佳时,医生应逐步增加单药剂量或药物种类。其中,利尿剂可被优先选用。当患者血压超过目标血压值20/10 mmHg时,联合用药可作为起始治疗。
该共识还特别强调了药物之间的相互作用,这一点对于老年人群尤其重要,此部分共识的制定基于老年人药代动力学改变,以及老年人群用药过多易致药物不良反应。
在老年高血压管理方面,仍有许多问题悬而未决,其中非常重要的一个问题为,是否所有老年高血压患者均可从降压治疗中获益?如何识别无法获益者?
未来的老年高血压临床和基础研究方向为老年高血压特征、靶器官损害机制、治疗策略和目标血压等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#专家共识#
42
#AHA#
49
#ACC#
45
#老年高血压#
38
#ACCF#
46