Cardiovasc Diabetol:冠心病对糖尿病患者左心室功能的不良影响
2022-03-03 Nebula MedSci原创
冠状动脉疾病对2型糖尿病患者的左心室收缩和舒张功能具有附加的有害影响。
冠状动脉疾病 (CAD) 在糖尿病患者中的发病率极高,是糖尿病患者的主要死亡原因。但是,迄今为止,在2型糖尿病 (T2DM) 患者中,冠状动脉疾病在左心室 (LV) 功能的累加效应中的作用尚未完全明确。
本研究旨在调查 CAD 如何影响 T2DM 患者的左心室收缩和舒张功能。
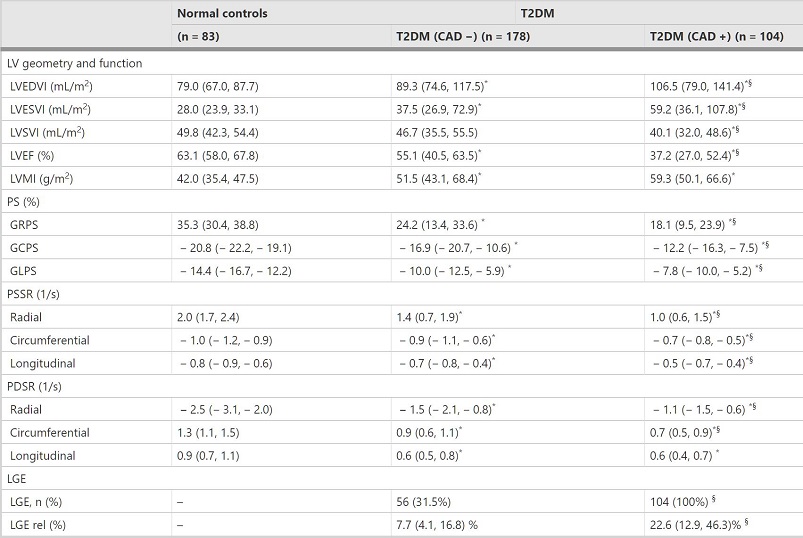
共招募了282位T2DM患者(其中104位合并CAD[CAD+],178位无CAD[CAD-])和83位性别和年龄相匹配的健康对照,予以心脏磁共振检查。测量每位受试者的LV结构、功能、全局应变 [包括径向、周向和纵向方向的收缩峰值应变 (PS)、收缩峰值 (PSSR) 和舒张应变率 (PDSR)] 和晚期钆增强 (LGE) 参数。根据 Gensini 评分(评估CAD的严重程度)的中位数将T2DM(CAD+)患者进一步分成两个亚组。构建多变量线性回归分析以明确降低左心室功能的决定因素。
三组受试者的心脏参数
与健康对照相比,T2DM(CAD-)患者的左室舒张末期和收缩末期容积指数增加,左室整体应变性降低;而T2DM (CAD+) 患者较T2DM (CAD-) 和健康对照组有显著的增加(左室舒张末期和收缩末期容积指数)和降低(左室整体应变性),除了纵向 PDSR (PDSR-L) (所有p<0.017)。
CAD对T2DM患者左心室收缩和舒张功能的影响
从Gensini 评分≤60的患者,到Gensini 评分>60的患者,除PDSR-L之外的左心室整体应变性的所有参数均表现出从正常对照组逐渐下降 (所有p<0.017)。CAD是2型糖尿病患者左心室的整体圆周PS (GCPS, β=0.22, p<0.001)、PSSR (PSSR-C, β=0.17, p=0.005)、PDSR (PDSR-C, β=0.22, p<0.001)、径向应变 PS (GRPS, β=0.19, p=0.001) 和整体纵向PS (GLPS, β=0.18, p=0.003) 降低的独立预测因子。最后,Gensini评分与合并CAD的2型糖尿病患者的GCPS、PSSR-C、PDSR-C、GRPS 和 GLPS降低均相关(所有p<0.05)。
综上所述,冠状动脉疾病对2型糖尿病患者的左心室收缩和舒张功能具有附加的有害影响。在T2DM (CAD+) 患者中,Gensini评分与左心室收缩和舒张功能降低有关。
原始出处:
Wang, J., Li, Y., Guo, YK. et al. The adverse impact of coronary artery disease on left ventricle systolic and diastolic function in patients with type 2 diabetes mellitus: a 3.0T CMR study. Cardiovasc Diabetol 21, 30 (2022). https://doi.org/10.1186/s12933-022-01467-y.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#DIA#
41
#BET#
29
#ASC#
32
学习学习
56
#左心室#
41
#糖尿病患者#
35