Neurology:左乙拉西坦使用时间对成人异柠檬酸脱氢酶野生型胶质母细胞瘤总生存率影响的观察研究
2021-10-29 Naomii MedSci原创
在整个标准放化疗方案中使用左乙拉西坦可能提高IDH-野生型胶质母细胞瘤患者的总体存活率。
胶质母细胞瘤,尤其是异柠檬酸脱氢酶(IDH)1型、2-野生型,是成人最常见的原发性恶性脑肿瘤。在可行前提下,最大限度的安全切除,然后标准的放化疗联合替莫唑胺是推荐的一线治疗方案。然而该方案生存益处有限,因此发现新的治疗靶点至关重要。替莫唑胺是一种口服烷化剂,可导致DNA甲基化,从而产生抗肿瘤下游效应。与O6-甲基鸟嘌呤-DNA甲基转移酶(MGMT)启动子甲基化相关的IDH-野生型胶质母细胞瘤对替莫唑胺更敏感,并与更好的预后相关。
在诊断时出现癫痫发作是弥漫性胶质瘤患者较长生存期的预测因子。这一临床观察似乎是矛盾的,因为癫痫和弥漫性胶质瘤都有共同的致病机制,并相互影响。此外,神经元活动已被证明促进胶质瘤的生长。第一种假设是,侵袭性较弱的弥漫性胶质瘤-预期存活时间更长-可能更有利于致痫过程的发展,这需要存活的神经元和可塑性。另一种解释是,针对共同致病机制的药物治疗可能同时影响癫痫发作和肿瘤控制。已有研究表明,几种抗癫痫药物,主要是丙戊酸钠、左乙拉西坦和培拉西坦,均具有抗肿瘤作用,替莫唑胺化疗可改善癫痫控制。在IDH-野生型胶质母细胞瘤患者中,癫痫发作的发生率高达30-60%,需要长期使用抗癫痫药物。因此,抗癫痫药物经常联合使用。左乙拉西坦(主要针对突触囊泡蛋白2A)已越来越多地被用作治疗胶质瘤相关癫痫的第一抗癫痫药物。由于其高治疗指数、有利的药代动力学、不与化疗药物相互作用、耐受性和止吐作用而导致的癫痫发作。
先前的研究表明,在标准联合放化疗方案与替莫唑胺联合治疗期间,使用左乙拉西坦与提高胶质母细胞瘤患者的存活率之间的关系,结果是相互矛盾的。然而,这些先前的研究没有系统地控制左乙拉西坦给药的持续时间(仅限于“基线”或“继续”)、IDH突变状态和MGMT启动子甲基化状态。近日,有研究调查了左乙拉西坦在标准联合放化疗方案和替莫唑胺联合应用期间的使用以及左乙拉西坦的持续时间(连续、部分时间或从不)是否影响成人IDH-野生型胶质母细胞瘤的同质单机构队列中的总存活率,并控制MGMT启动子甲基化状态。
观察性单机构队列研究(2010-2018年)。纳入标准为:1)患者≥,年龄18岁;2)新诊断的幕上肿瘤;3)IDH-野生型胶质母细胞瘤的组织分子诊断;4)标准放化疗方案。为了评估标准放化疗期间使用左乙拉西坦的生存益处(全程、部分时间和从不分组),建立了Cox比例风险模型。根据性别、年龄、确诊时癫痫发作、RTOG-RPA分级、肿瘤位置、术前体积、切除范围和O6-甲基鸟嘌呤-DNA甲基转移酶启动子甲基化状态,我们对在标准放化疗方案的整个过程中使用左乙拉西坦的患者和部分使用或从不使用左乙拉西坦的患者进行了病例配对分析(1:1),这些标准包括:性别、年龄、确诊时癫痫发作、RTOG-RPA分级、肿瘤位置、术前体积、切除范围和O6-甲基鸟嘌呤-DNA甲基转移酶启动子甲基化状态。排除O6-甲基鸟嘌呤-DNA甲基转移酶启动子甲基化状态不可用的患者(48.5%)。
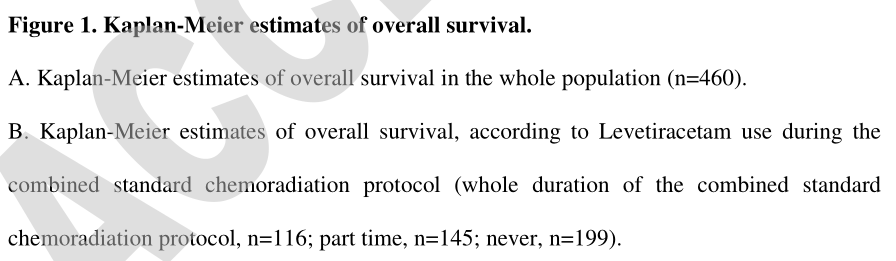
- 纳入460例患者。在标准放化疗方案的整个过程中,116名使用左乙拉西坦的患者的中位总生存期(21.0个月;95%CI,17.2-24.0)比126名同时使用左乙拉西坦的患者(16.8个月;95%CI,12.4-19.0)和218名从未使用左乙拉西坦的患者(16.8个月;95%CI,12.4-19.0)要长接受左乙拉西坦治疗(16.0个月;95%可信区间15.5~19.4;p=0.027)。
- 在标准放化疗方案的整个过程中使用左乙拉西坦(调整后的危险比为0.69;95%CI为0.52-0.93;p=0.014)、O6-甲基鸟嘌呤-DNA甲基转移酶启动子甲基化(AHR0.53;95%CI为0.39-0.71;p<0.001)和大体肿瘤切除(AHR0.57;95%CI为0.44-0.74;p<0.001)是较长总生存期的独立预测因素。
- 病例匹配后(每组54例),在标准放化疗方案的整个过程中使用左乙拉西坦的总生存期较长(HR=0.63;95%CI,0.42-0.94,p=0.023)。
在整个标准放化疗方案中使用左乙拉西坦可能提高IDH-野生型胶质母细胞瘤患者的总体存活率。在未来多中心试验的抗肿瘤策略中应考虑到这一点。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
27
#胶质母细胞#
41
#母细胞瘤#
47
#野生型#
52
#观察研究#
47
#生存率#
27
#细胞瘤#
42
#柠檬酸#
41