MOL CELL:人乳腺癌细胞中细胞因子介导的内分泌抗药性的结构及分子机制
2017-03-25 MedSci MedSci原创
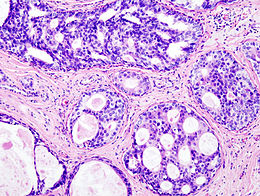
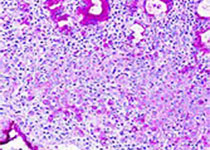
一项研究表明ERα是乳腺癌细胞中促炎细胞因子的信号通路的效应子,IL1β和TNFα能增加依赖于ERα的乳腺癌侵袭,细胞因子通过S305的IKKβ磷酸化激活未形成配体的ERα,Phospho-S305导致ERα和他莫昔芬抗性的结构变化。
最近,来自加利福尼亚大学细胞与分子医学系的研究人员报道了一项关于人乳腺癌细胞中细胞因子介导的内分泌抗药性的结构及分子机制的研究,相关研究刊登于国际杂志MOL CELL上。
研究表明ERα是乳腺癌细胞中促炎细胞因子的信号通路的效应子,IL1β和TNFα能增加依赖于ERα的乳腺癌侵袭,细胞因子通过S305的IKKβ磷酸化激活未形成配体的ERα,Phospho-S305导致ERα和他莫昔芬抗性的结构变化。
原始出处:
Joshua
D. Stender, Jerome C. Nwachukwu, Irida Kastrati. et al.Structural and Molecular Mechanisms of Cytokine-Mediated Endocrine
Resistance in Human Breast Cancer Cells. DOI:
http://sci-hub.cc/10.1016/j.molcel.2017.02.008 |
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
47
#分泌#
38
#CEL#
47
#胞因子#
40
#癌细胞#
42
#细胞因子#
29
#抗药性#
33