护士主导的电子健康护理干预措施能够改善冠心病患者预后
2021-09-07 MedSci原创 MedSci原创
护士主导的电子健康心脏康复计划对改变行为风险因素及提高健康相关生活质量有效。
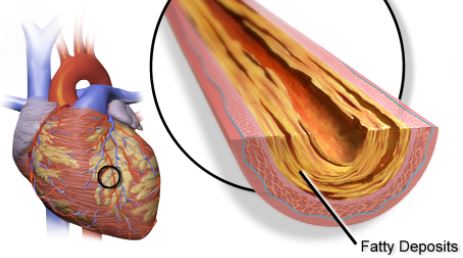
冠心病是中老年人的常见病,多发病,严重危及人们生命安全。大约75%的冠心病能够通过改变行为和管理危险因素得到预防,如缺乏运动、不健康饮食、吸烟和心理问题。
尽管心脏康复治疗可以有效促进患者健康的生活方式,提高生活质量,降低心脏病相关的发病率和死亡率,在改善冠心病的危险因素和延缓疾病进展方面有明显的健康效益,但患者对心脏康复治疗的接纳程度和依从性仍不理想。
近日,发表在International Journal of Nursing Studies杂志的一篇文章探索了护士主导的电子健康心脏康复计划对成年冠心病患者健康行为,自我效能感,焦虑和抑郁,健康相关生活质量,生理风险参数以及非计划性使用卫生服务的影响。

这项研究采用单盲、随机对照研究设计,随机分配146名住院患者接受护士主导的电子健康心脏康复计划干预或常规护理。基于社会认知理论,护士当面了解患者的个体化需求,设定目标并制定行动计划,以改善行为风险因素并让病人学会利用信息和通信技术平台接受心脏康复治疗。出院后,该电子平台能够帮助患者获得疾病健康管理知识,并监测健康行为改变的目标达成情况。护士每周通过微信平台以小组形式就病人的目标实现和生活方式改变提供反馈,从而增加同行影响力。分别在基线和干预后6周和12周,收集患者健康行为、生理风险参数和临床结局的相关数据。

干预后6周,与对照组相比,干预组每天行走步数(β=2628.48,p= 0.022)、每周静坐时间(β=-640.30,p= 0.006)和健康行为(β=25.17,p < 0.001)均有显著改善。干预后12周,每天步数(β=2520.00,p=0.006)、每周静坐时间(β =-719.73,p= 0.004)和健康行为(β=16.09,p < .001)持续改善。自我效能感(β=0.61,p=0.005)和健康相关生活质量(标准差=0.56,p<0.001)方面,干预组显著优于对照组。
研究结果显示出护士主导的电子健康心脏康复计划对改变行为风险因素及提高健康相关生活质量的有效性。这些发现也为应用电子健康护理干预措施促进冠心病患者康复提供思路。
原文出处:
Jing Jing Su, Doris Sau-fung Yu, Effects of a nurse-led eHealth cardiac rehabilitation programme on health outcomes of patients with coronary heart disease: A randomised controlled trial, International Journal of Nursing Studies, https://doi.org/10.1016/j.ijnurstu.2021.104040.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#干预措施#
40
#患者预后#
30
#冠心病患者#
60
护理很重要
62
#心血管#
73
厉害
60
研究设计很棒,值得借鉴
63
漂亮
53