JTO:淋巴细胞浸润、PD-L1、吸烟史之间是何种微妙关系,它们如何影响未曾接受免疫抑制剂治疗的非小细胞肺癌患者的预后?
2019-02-08 良医汇-肿瘤医生APP 肿瘤资讯
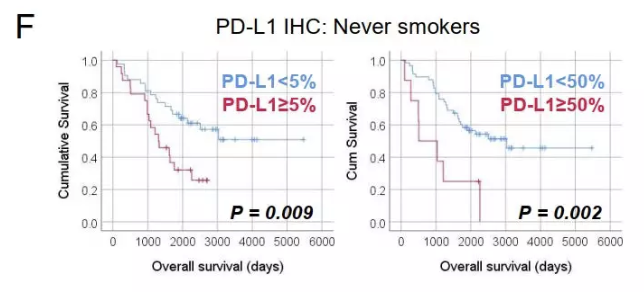
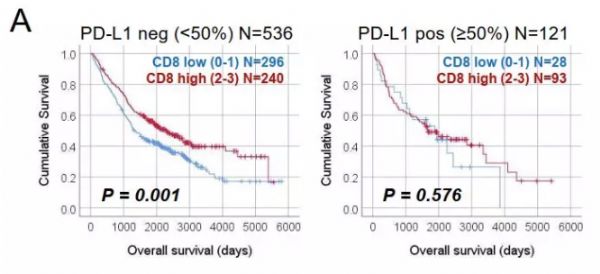
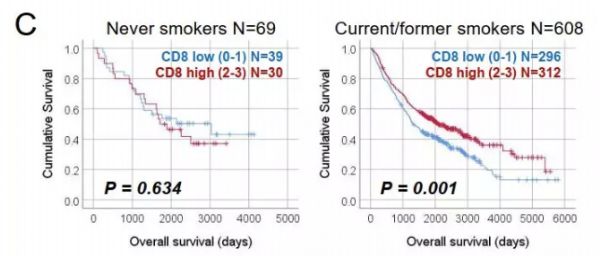
肿瘤的发展依赖于肿瘤细胞与周围间质细胞之间的相互作用。抗肿瘤免疫治疗需要多种免疫细胞参与其中。因此,将更多的免疫细胞标志物纳入研究对于预测非小细胞肺癌(NSCLC)患者的预后至关重要。T细胞和B细胞/浆细胞浸润与NSCLC患者预后相关,但在PD-L1阳性患者中未评估过它们之间的相关性。一项回顾性研究分析了在未接受PD-1/PD-L1抑制剂治疗的两个NSCLC患者队列中淋巴细胞浸润和PD-L1表达与

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#抑制剂#
39
#非小细胞#
28
#肺癌患者#
35
#PD-L1#
34
#免疫抑制剂#
34
#淋巴细胞#
38
#非小细胞肺癌患者#
26