基于右心室功能的肺动脉高压患者无创风险预测
2021-11-18 刘少飞 MedSci原创
右心室功能障碍是肺动脉高压 (PAH) 结局的主要决定因素。我们旨在确定与不良结果相关的超声心动图右心参数,并为 PAH 患者开发一种基于超声心动图的无创风险评分。
肺动脉高压(PAH)是一种罕见且严重的慢性肺部疾病,可导致右心衰竭和过早死亡。尽管在过去 20 年中,新的治疗干预措施改善了临床管理,但 PAH 仍与高发病率和死亡率相关。因此,精确的个体风险评估对于识别有风险的患者并根据疾病严重程度和预后调整治疗至关重要。
综合风险评估工具已在过去几年发布,包括各种临床、功能和血流动力学变量。 2015 年 ESC/ERS 肺动脉高压 (PH) 指南引入了一种风险评估工具来预测一年死亡率,允许将个体分为低(<5%)、中(5-10%)和高风险(>10 %) 类别。该模型中的风险评估基于临床恶化、功能性肺活量、脑钠肽 (BNP) 或 N-末端-proBNP (NT-proBNP) 浓度、侵入性血流动力学变量以及右心房 (RA) 区域的超声心动图评估和心包积液。由于 ESC/ERS 风险评分需要广泛的临床和侵入性评估,COMPERA、SPAHR 或法国注册等进一步的注册研究试图开发该风险工具的简化版本,将预测因子的数量从 12 个减少到 8 个或更少。相比之下,REVEAL-Study 提出了一个风险方程,其中包含额外的变量,包括生命体征和肾功能损害,以预测 PAH 患者的不良结果。
右心室 (RV) 功能障碍是 PAH 结局的主要决定因素,但这些风险模型不能很好地代表 RV 功能的超声心动图参数。三尖瓣环平面收缩期偏移 (TAPSE) 的减少与 PAH 的生存率呈负相关。其他参数如 RA 扩张和心包积液也被证明可以预测 PAH 的预后。同样,右侧纵向峰值应变被确定为 PAH 患者全因死亡率的预测因子。相对较小的样本量、有限的随访和对混合人群(包括 PAH 以及其他形式的 PH)的分析是可用数据的局限性。
专家认为,将右心室参数整合到 PAH 患者的风险评估中是改善护理的机会。因此,我们在一个特征一致的当代 PAH 患者临床队列中研究了右心功能障碍的超声心动图参数的预后价值。
研究队列:
在一项回顾性队列研究中,我们连续纳入了 254 名于 2010 年至 2018 年在汉堡-埃彭多夫大学医学中心门诊就诊的 PAH 患者。 PAH 的诊断基于当前指南,由右心导管插入术引起,需要平均肺动脉压≥25 毫米汞柱且肺动脉楔压≤15 毫米汞柱。该队列由患有流行病的患者和新诊断的患者组成。18 岁以下的患者被排除在进一步分析之外。
收集了临床、实验室、肺功能和超声心动图数据。临床评估包括人口统计学、重要参数、体重指数 (BMI) 和 PAH 特异性药物。实验室测量包括 NT-proBNP、血清肌酐和估计的肾小球滤过率 (eGFR) 值。功能评估包括 WHO 功能等级、标准化的 6 分钟步行测试和肺功能测试,包括肺一氧化碳扩散能力 (DLCO) 和用力肺活量 (FVC)。
研究队列患者特征:
在纳入分析的 254 名患者中,33.9% 为女性,中位年龄为 65.5 岁 (49.4, 74)。收缩压为 128 mmHg (SD ± 22.8)。大多数患者为 WHO 功能等级 III 或 IV,并且 6MWD 严重降低(269.2 m,SD ±183.9)。肺功能测试显示 DLCO 为 58% (38.9, 77),FVC 为 75% (58, 86)。大多数患者的 NT-proBNP 浓度升高 >300 pg/mL,39% 的患者肾功能受损,eGFR 低于 60 mL/min/1.73 m 2. 在 23.2% 的患者中,没有建立 PAH 特异性治疗,48% 接受单一疗法,28.7% 接受两种或更多不同药物的联合治疗。在这些患者中,45% 患有动脉高血压,16.5% 被诊断患有糖尿病,20.5% 患有预先存在的冠状动脉疾病,3.6% 患有外周动脉疾病。
超声心动图参数
大多数患者的 RA 区域扩大,与参考值相比,RV 底部和 RV 内侧尺寸显着扩大。RV的纵向直径在正常范围内。在 14 个人中检测到心包积液。大多数队列中 RV 功能受损,表现为 FAC 减少、TAPSE 减少和 RV 游离壁应变受损。
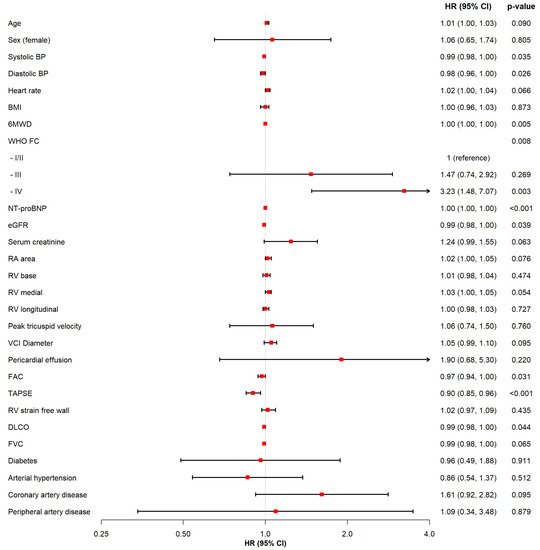
回归分析
在 4.18 年的中位随访期间,63 名(24.8%)患者死亡,11 名(4.3%)患者接受肺移植,复合终点的发生率为 25.3/1000 人年。在单变量 Cox 回归分析中,以下参数与复合终点相关:低收缩压、WHO 功能 IV 级、较低的 6MWD、NT-proBNP 浓度、肾功能损害、DLCO 受影响、TAPSE 减少和 FAC 减少。
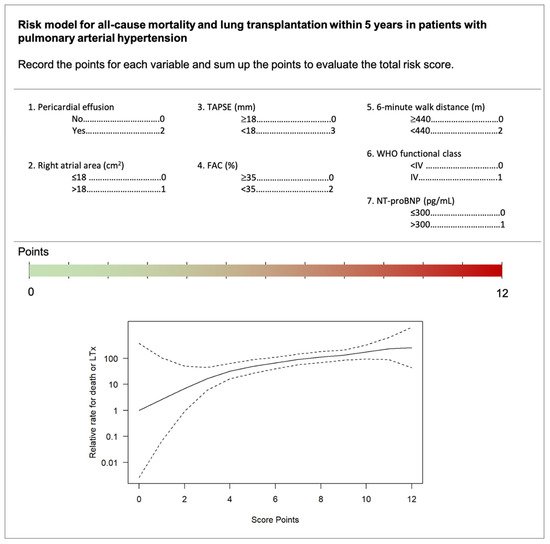
无创风险评分
基于模型 2 的多变量结果,每个预测变量都被分配到一个分数。NT-proBNP 浓度 >300 pg/mL、WHO 功能等级 IV 和 RA 面积 >18 cm 2被指定为 1 分。存在心包积液、6MWD < 440 m 和 FAC < 35% 记为 2 分。TAPSE <18 mm 作为主要预测指标由三个点表示。可以将每个变量的点相加以显示总风险。最终风险评分范围为 0 到 12 分,而数字越大表示风险越高。
研究结论:
该研究分析了 254 名 PAH 患者的功能状态、实验室结果和超声心动图参数。我们包括这些参数以使用 Cox 回归模型估计全因死亡或肺移植。分析包括使用指南推荐变量的传统模型和扩展的超声心动图模型。根据最终模型得出 12 分风险评分,表明与五年内主要结局的关联。中位随访时间为 4。2年74例患者死亡或接受肺移植。传统模型的 C 指数为 0.539,而扩展的超声心动图模型提高了辨别力(C 指数 0.639,p值 0.017)。最终,新开发的风险评分包括 WHO 功能等级、6 分钟步行距离、N 端脑钠肽浓度、心包积液、右心房面积、三尖瓣环平面收缩期偏移和面积分数变化。
研究启示:
整合超声心动图评估的右心功能可提高 PAH 患者死亡或肺移植的预测。有必要对这一发现进行独立验证。
文献出处:
Qaderi V, Weimann J, Harbaum L, Schrage BN, Knappe D, Hennigs JK, Sinning C, Schnabel RB, Blankenberg S, Kirchhof P, Klose H, Magnussen C. Non-Invasive Risk Prediction Based on Right Ventricular Function in Patients with Pulmonary Arterial Hypertension. J Clin Med. 2021 Oct 31;10(21):5130. doi: 10.3390/jcm10215130. PMID: 34768652; PMCID: PMC8584811.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肺动脉高压患者#
51
#动脉高压#
36
#右心室功能#
37
#风险预测#
50
#右心室#
49