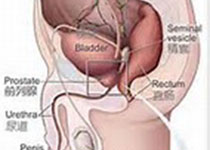
Prostate Cancer P D:术前提高的中性粒细胞-淋巴细胞比例预示着根治性前列腺切除术的升级
2017-12-20 AlexYang MedSci原创
中性粒细胞-淋巴细胞比例(NLR)是全身性炎症反应的一个广泛使用的、代表性的标记。NLR可以从简单的、廉价的外周血样中计算出。高的NLR是许多恶性肿瘤,包括泌尿肿瘤的一个消极预后因素。最近,有研究人员评估了术前接受根治性前列腺切除术(RP)病人中的NRL对局部前列腺癌(PCa)的预后价值。研究包括了7425名病人的记录,并对其进行了回顾性的分析,并根据ROC分析和之前的文献,NLR的截断点为3。研
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
42
#细胞比例#
48
#Prostate Ca#
31
#前列腺切除#
45
#PRO#
30
#根治#
31
#ROS#
31
#淋巴细胞#
19
#中性粒细胞#
22
好文章.谢谢分享!
52