PLoS One:CHADS2和CHA2DS2-VASc评分可用于血液透析患者的死亡的预测
2016-07-11 phylis 译 MedSci原创
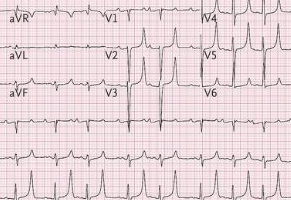
背景:CHADS2和CHA2DS2-VASc评分通常用于房颤患者预测卒中的发生,和Charlson合并症指数(CCI)量表常用于发病率的评估。在血液透析患者死亡率的评分系统及比较尚不清楚。研究者旨在评估CHADS2,CHA2DS2-VASc和CCI分数预测血液透析患者的死亡率。方法:利用台湾国家健康保险系统数据(NHIRD)中, 2005年1月号到 2009年12月31,超过20岁开始血液透析的患
背景:CHADS2和CHA2DS2-VASc评分通常用于房颤患者预测卒中的发生,和Charlson合并症指数(CCI)量表常用于发病率的评估。在血液透析患者死亡率的评分系统及比较尚不清楚。研究者旨在评估CHADS2,CHA2DS2-VASc和CCI分数预测血液透析患者的死亡率。
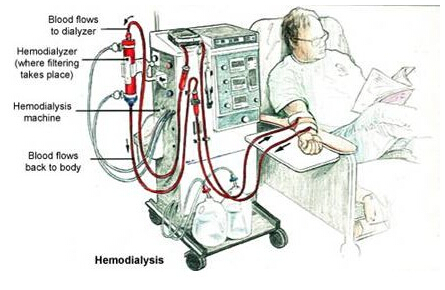
方法:利用台湾国家健康保险系统数据(NHIRD)中, 2005年1月号到 2009年12月31,超过20岁开始血液透析的患者及接受透析超过3个月纳入研究。排除肾移植术后透析或帕金森氏症患者。研究者根据ICD-9编码和分类计算CHADS2评分,CHA2DS2-VASc评分及CCI评分,将患者分为三组: 0-1分,2-3分,超过4分。从NHIRD共纳入3046名血液透析患者,评估各个评分系统(CHADS2评分,CHA2DS2-VASc评分,和CCI评分)与死亡率的相关性。
结果:CHADS2和CHA2DS2-VASc评分对总死亡率有良好的预测值(CHADS2 AUC = 0.805;CHA2DS2-VASc AUC = 0.790)。然而,CCI得分并没有显示出类似的结果(AUC = 0.576)。
结论:研究结果表明,CHADS2和CHA2DS2-VASc评分可用于血液透析患者的死亡的预测。
原始出处:
Yang H, Chen YH, et al. Prediction of Mortality in Incident Hemodialysis Patients: A Validation and Comparison of CHADS2, CHA2DS2, and CCI Scores. PLoS One. 2016 May 5
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









好想看一下评分表的内容
68
#CHA2DS2-VASc评分#
58
#Plos one#
44
#ADS#
47
#CHA2#
43
好文值得点赞!继续关注学习。
75
#ASC#
34
#血液透析#
37
#透析患者#
53
#CHA2DS2-VASc#
42