JAMA:GCK突变者血糖高但血管并发症发生率较低
2014-01-21 孙云 编辑 中国医学论坛报
一项英国研究显示,尽管葡萄糖激酶(GCK)突变者自出生后空腹血糖水平即轻度升高,但此人群发生微血管和大血管并发症的几率较低。文章1月15日在线发表于《美国医学会杂志》(JAMA)。 研究纳入99例携带GCK突变基因的受试者、91例无糖尿病无基因突变的对照者和83例早发2型糖尿病患者(诊断糖尿病时年龄为45岁或更小)。结果显示,这三组患者的平均糖化血红蛋白(HbA1c)分别为6.9
一项英国研究显示,尽管葡萄糖激酶(GCK)突变者自出生后空腹血糖水平即轻度升高,但此人群发生微血管和大血管并发症的几率较低。文章1月15日在线发表于《美国医学会杂志》(JAMA)。
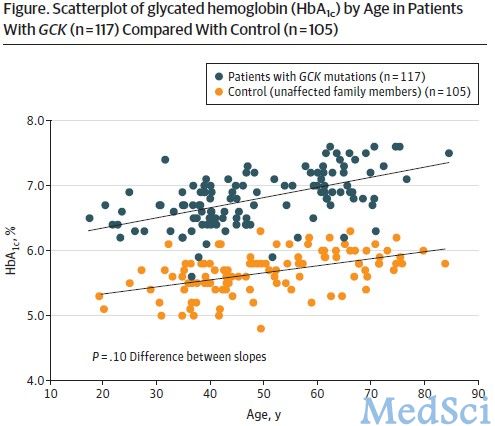
研究纳入99例携带GCK突变基因的受试者、91例无糖尿病无基因突变的对照者和83例早发2型糖尿病患者(诊断糖尿病时年龄为45岁或更小)。结果显示,这三组患者的平均糖化血红蛋白(HbA1c)分别为6.9%、5.8%和7.8%。GCK突变者微血管和大血管并发症的发生率(分别为1%和4%)与对照组(2%、11%)相似,且明显低于2型糖尿病患者(36%、30%)。
原文出处:
Steele AM1, Shields BM1, Wensley KJ1, Colclough K2, Ellard S3, Hattersley AT1.Prevalence of vascular complications among patients with glucokinase mutations and prolonged, mild hyperglycemia.JAMA. 2014 Jan 15;311(3):279-86. doi: 10.1001/jama.2013.283980. 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#发生率#
42
#并发#
45
#血管并发症#
43