脑出血的八大先兆表现
2016-08-15 脑血管病预防与治疗 脑血管病预防与治疗
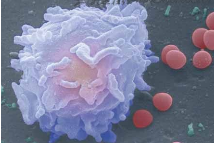
脑出血是指非外伤性脑实质内血管破裂引起的出血,最常见的病因是高血压、脑动脉硬化、颅内血管畸形等,常因用力、情绪激动等因素诱发,故大多在活动中突然发病,临床上主要表现为意识障碍、肢体偏瘫、失语等神经系统的损害。脑出血起病急骤、病情凶险、死亡率非常高,往往会在数小时或几天之内夺走患者的生命,是目前中老年人致死性疾病之一。但脑出血还是有其逐步发展演变的过程,50% 的患者在起病初期会或多或少表现出一些异
脑出血是指非外伤性脑实质内血管破裂引起的出血,最常见的病因是高血压、脑动脉硬化、颅内血管畸形等,常因用力、情绪激动等因素诱发,故大多在活动中突然发病,临床上主要表现为意识障碍、肢体偏瘫、失语等神经系统的损害。
脑出血起病急骤、病情凶险、死亡率非常高,往往会在数小时或几天之内夺走患者的生命,是目前中老年人致死性疾病之一。但脑出血还是有其逐步发展演变的过程,50% 的患者在起病初期会或多或少表现出一些异常情况,即出现一些有预兆的前驱表现。
先兆症状出现后的第一年内发生脑出血的危险性很大,尤其在两个月内最为危险。一旦出现这些先兆表现,就预示着脑出血即将发生,或已是脑出血的前驱阶段。这时如能仔细观察,就能及时发现异常,并到医院争分夺秒地进行治疗,从而控制疾病发展,避免严重后果。
脑出血的先兆表现有哪些呢?
1、经常出现反复性的流鼻血。
2、突然发作较为剧烈的头痛(与通常性质头痛不一样,呈头炸裂样),或病程较长,有逐渐加重的趋势;并多伴有恶心、呕吐的症状表现。
3、颈部变得僵直,后枕部不适(活动受限,尤其是低头,下颌抵上胸动作困难)。
4、出现头晕的症状,感到周围环境不停旋转,无法稳定的站立或是晕倒在地。这些表现可是一过性的,也可反复出现或是愈发严重。
5、暂性视物模糊,或眼睛有重影出现,以后可自行恢复正常,或出现失明。
6、突然感到一侧身体麻木、无力、活动不便,手持物掉落,嘴歪、流涎,走路不稳。
7、和他人交谈时突然出现语言障碍,或口齿不清,听不懂别人所说的话。
8、走路不稳定,意识出现障碍,反应差,甚至神志不清醒,大小便失禁。
现代生活节奏加快,使脑血管疾病发病率明显增加,如果此时大脑血管出现险情,大脑供血供氧不足,可有困倦、乏力症状。此外,还会有手指麻木、原因不明跌倒、精神状态发生变化等前兆。
当上述先兆症状出现时,患者在思想上既要高度重视,又不能过度紧张以致惊慌失措。情绪要镇静,避免因血压波动而加重病情。应尽快将患者送到医院就诊,并详细告诉医生已出现的预兆表现,以便明确诊断,及时治疗。
这些先兆可能是缺血性卒中或出血性卒中,其判断需专业医生的介入。如果你或你的亲人、朋友、同事在日常生活中出现了上述症状表现中的一个或几个(不会是全部),一定要在第一时间到医院进行专业的诊断,以免脑出血的突然来袭。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












继续关注
66
继续学习
68
继续关注
62
继续学习
57
继续关注
80
好好学习一下
41