J RENAL NUTR:基于共识的血液透析环境中高钾血症管理建议
2022-07-09 liangying MedSci原创
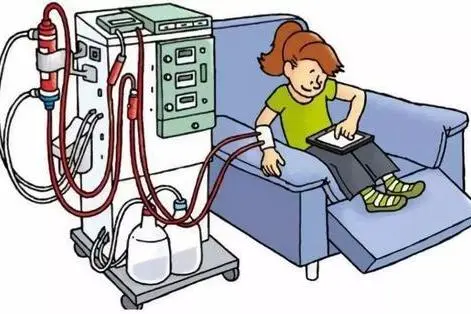
血液透析环境中高钾血症的治疗是复杂的,需要根据患者的具体情况做出决定。
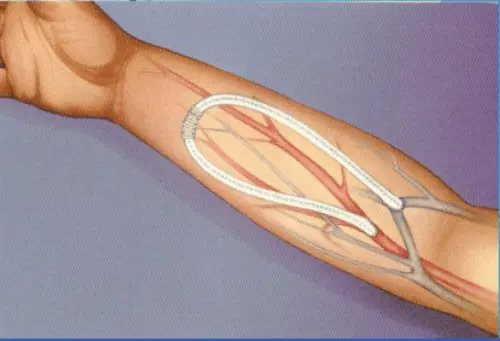
高钾血症,通常定义为血清钾>5.0 mmol/L或>5.5 mmol/L,是在慢性肾病(CKD)晚期患者中观察到的常见电解质紊乱,与心律失常风险增加有关。近三分之二接受血液透析的患者在长时间透析间期后出现高钾血症(K+>5.5 mmol/L)。目前的国际指南不能反映血液透析患者高钾血症处理的最新证据,而且在这一领域缺乏高质量的已发表的研究。本共识指南旨在提供与临床实践相关的建议。
研究者通过系统的文献综述对现有已发表的证据进行了评估,并使用冠名组技术从经验丰富的肾病学家小组中商讨出共识建议,包括监测、饮食限制、K+结合剂处方以及伴随处方肾素-血管紧张素-醛固酮系统抑制剂。
在本系统文献综述的更新中,对MEDLINE和Cochrane图书馆的初步搜索返回了429条独特引文。在筛选一组确定的合格标准(补充图1)后,纳入了38份报告成人高钾血症药理学或非药理学治疗的干预性或观察性研究的合格记录(补充表3)。其中,有10份出版物,涵盖了9项独特的研究,调查了血液透析环境中的高钾血症。
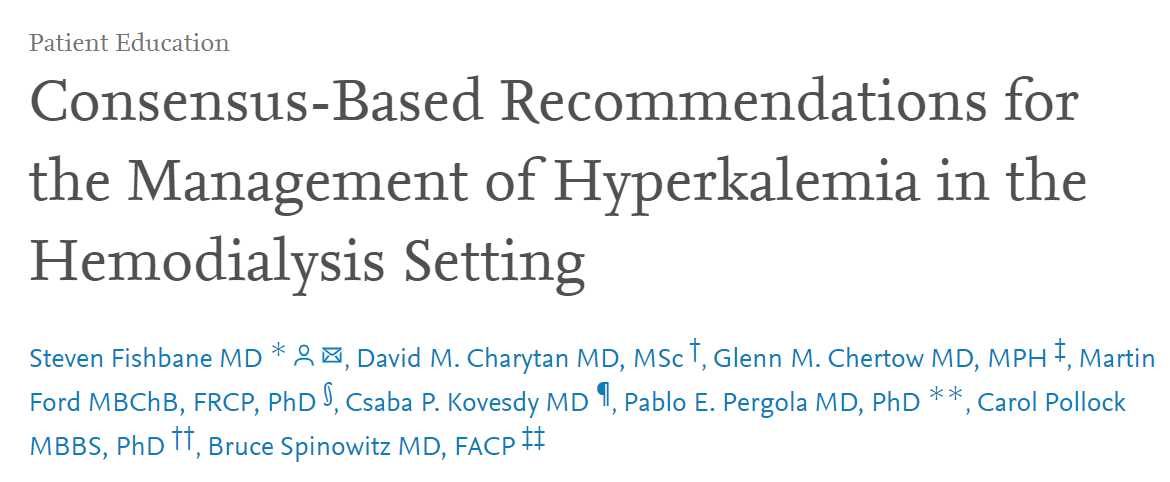
关于CKD患者高钾血症监测的建议在很大程度上是间接的,没有证据表明血液透析设置的理想时机或频率。当在周五而不是周一或周三(对于周一-周三-周五时间表的患者)进行测量时,观察到血清K+(5.5 mmol/L)升高与住院之间的相关性更强。根据小组成员的经验,在整个医疗系统中,周中进行测量是最常见的做法。
血液透析环境中监测K+的共识声明
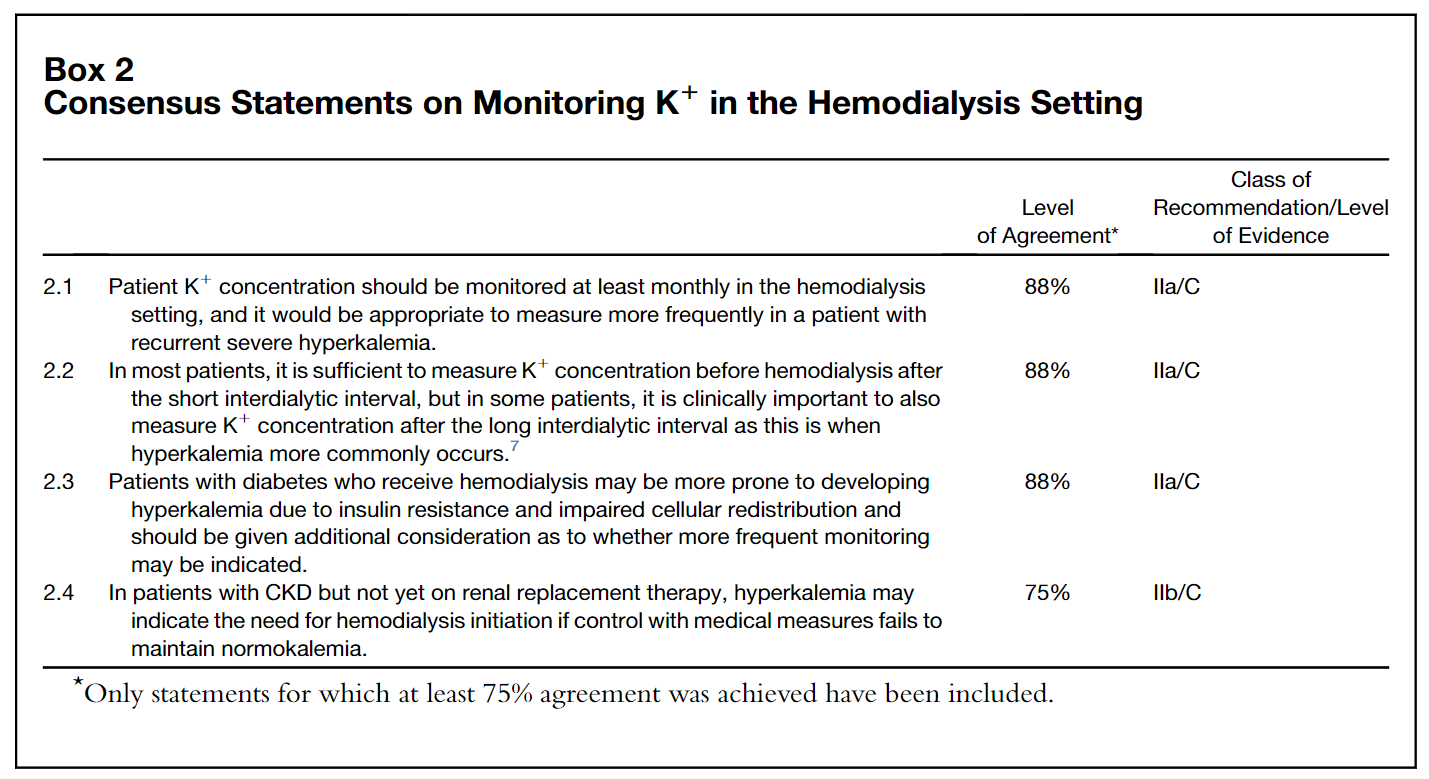
在评估推荐的饮食K+限制的效果时,还需要进一步考虑患者的依从性水平和患者的生活质量(QoL)。考虑到处方K+结合剂后调整患者饮食的潜力,专家组断言,有限的证据表明低K+饮食与血液透析患者血清K+的减少有关;也没有证据表明放宽K+限制是安全的。专家组一致认为,在没有咨询肾病专家和其他医疗服务提供者之前,建议患者不要放松膳食K+摄入量是很重要的,因为增加膳食K+可能会干扰K+粘合剂处方的目的。
维持性血液透析患者饮食K+限制的共识声明
总的来说,虽然K+结合剂可降低高钾血症的发生率,但还需要进一步的证据,包括减少K+饮食或K+结合剂治疗是否能改善以患者为中心的结果。血液透析环境中高钾血症的治疗是复杂的,需要根据患者的具体情况做出决定。
参考文献:Steven Fishbane, David M. Charytan, Glenn M. Chertow, et al, Consensus-Based Recommendations for the Management of Hyperkalemia in the Hemodialysis Setting, Journal of Renal Nutrition, Volume 32, Issue 4, 2022, Pages e1-e14, ISSN 1051-2276, https://doi.org/10.1053/j.jrn.2021.06.003.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#renal#
57
#血液透析#
49
#高钾#
43
学习了,谢谢分享
52
好的,学习了,以后有机会学习
60