Oncolmmunology:化普通为神奇:β-受体阻滞剂助免疫治疗一臂之力
2018-01-21 慧语 肿瘤资讯
免疫疗法虽然为癌症的治疗提供了更多选择,但其疗效仅对部分患者有效。
免疫疗法虽然为癌症的治疗提供了更多选择,但其疗效仅对部分患者有效。宾夕法尼亚州立大学的研究人员在临床实践中发现,接受免疫治疗且同时服用β受体阻滞剂(如:Propranolol心得安)的转移性黑色素瘤患者比那些仅单独接受免疫治疗的患者总生存率更高。在此基础上,研究人员对临床数据进行了回顾性分析,并在小鼠实验中得到了验证。这项新研究成果近期发表在《OncoImmunology》。
背景
肿瘤患者如果合并有心血管疾病,医生通常会为患者开具β受体阻滞剂药物。一些研究报道指出乳腺癌和卵巢癌患者使用β受体阻滞剂药物后的生存状况更好,那么β受体阻滞剂能否提高免疫治疗的疗效呢?理论上似乎可行,因为阻断β受体信号有助于抑制肿瘤细胞的增殖、迁移和肿瘤组织中血管形成,同时还会使具有效应表型的CD8+T细胞在肿瘤内增加,以此改善免疫功能。
方法
1、回顾性临床数据收集
2000年1月1日至2015年3月31日期间,接受IL-2,aPD-1和/或CTLA-4免疫治疗的晚期黑色素瘤成年患者。收集的变量包括免疫治疗开始时的年龄、性别、疾病分期以及β受体阻滞剂的使用等。其中β受体阻滞剂使用可以分为两种情况:β1选择性阻滞剂(β1-blocker,阿替洛尔,艾司洛尔和美托洛尔)和β受体阻滞剂(Pan β-blocker,Propranolol心得安)。
2、小鼠肿瘤模型制备和治疗方案
肿瘤植入6-8周大的雌鼠体内后,每天监测以确定肿瘤体积。肿瘤接种后6-9天左右(肿瘤体积在20-100mm 3),随机将小鼠分入各治疗组。所有的处理均为腹膜内给药,无菌PBS作为对照注射。IL-2以120,000IU每天两次施用,持续两天,间隔两天;aPD-1组分别在第1,4,8,11,15,18天给药6次,每次200mg剂量。β受体阻滞剂并按Propranolol(10mg/kg)浓度每日给药连续3周。在治疗开始,每两天测量一次肿瘤体积直至大于1000mm3后再每天进行测量,肿瘤体积计算公式为长*宽*高/2(用数字卡尺测量,单位mm3)。生存分析的终点事件包括肿瘤体积大于1500mm 3、小鼠昏睡以及出现导致小鼠无法运动的腹水。
结果
1、β受体阻滞剂延长免疫治疗的转移性黑色素瘤患者生存
共计纳入接受免疫治疗(包括白细胞介素IL-2,CTLA4抑制剂和PD-1/PD-L1抑制剂)治疗的195位转移性黑素瘤患者,分为3组:接受β1受体阻滞剂治疗组(n=17);服用β1选择性阻滞剂组(n=45)和无β受体阻滞剂组(n=133)。总体5年存活率在β受体阻滞剂治疗组(Pan β-blocker)为70%,而β1选择性阻断剂组(β1-blocker)和无β受体阻滞剂组(no β-blocker)仅为25%(图1)。
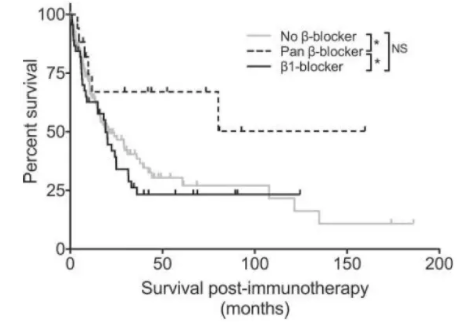
图1 接受β受体阻滞剂的恶性黑色素瘤患者延长免疫治疗后存活
2、β受体阻滞剂提高免疫疗法在临床前黑色素瘤动物模型的抗肿瘤能力
研究者制备了一个平行的小鼠模型。荷瘤小鼠每天接受10mg/kg的β受体阻断剂心得安Propranolol治疗三周,和/或每周两次200mg PD-1连续三周/或每天两次120,000IU IL-2持续五天,两个周期。(图2)
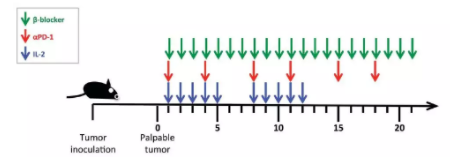
图2 动物模型给药模式
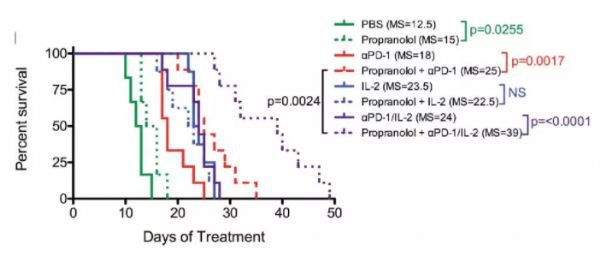
小鼠的生存分析显示,单独使用β受体阻滞剂组没有生存获益(Propranolol组中位生存时间为15天),Propranolol不能改善IL-2治疗患者的生存(Propranolol+IL-2组中位生存时间23.5)。然而,Propranolol显着延长了PD-1抑制剂治疗的的小鼠的存活时间(单纯PD-1组中位生存时间18天,Propranolol+PD-1组中位生存时间25天)。Propranolol联合aPD-1/IL-2组的存活率显着延长,中位生存时间为39天(图3)。
图3 不同治疗组的小鼠黑色素瘤模型的生存曲线
结论和点评
综上,本研究揭示β受体阻滞剂有效地增强了基于PD-1免疫疗法的抗肿瘤活性,且β受体阻滞剂与PD-1/IL-2的组合是最有效的,表明β受体阻滞剂可能是通过多种机制来改善预后的。此结果为晚期黑色素瘤治疗提供了新的信息,有望扩大免疫治疗的获益人群。本研究仅是基于回顾性数据的分析和动物模型的验证,证据级别有限,能否影响临床实践还需要前瞻性研究的进一步确证。本研究的作者Drabick博士目前正在开展一项前瞻性临床试验--接受帕姆单抗一线治疗同时使用Propranolol是否会提高转移性黑色素瘤患者的预后。
原始出处:
Kathleen M. Kokolus, et al. Beta blocker use correlates with better overall survival in metastatic melanoma patients and improves the efficacy of immunotherapies in mice. OncoImmunology, Dec 2017.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#受体阻滞剂#
30
#阻滞剂#
41
#Oncol#
32
不错的文章不错的文章
69
不错的文章不错的文章
63
不错的文章不错的文章
74
#β-受体阻滞剂#
40
是很好的学习材料.不错.以后会多学习.
71
免疫疗法虽然为癌症的治疗提供了更多选择.但其疗效仅对部分患者有效.宾夕法尼亚州立大学的研究人员在临床实践中发现.接受免疫治疗且同时服用β受体阻滞剂(如:Propranolol心得安)的转移性黑色素瘤患者比那些仅单独接受免疫治疗的患者总生存率更高
58