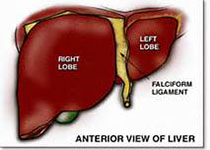
Sci Trans Med:乙肝新药进入临床阶段,有望彻底治愈乙肝
2017-11-07 佚名 medicalxpress
德州生物医学研究所西南国家灵长类动物研究中心(SNPRC)的研究人员们开始了慢性乙型肝炎病毒(HBV)新药的临床试验。测试结果显示,这种新颖的治疗方法和药物传递机制是安全有效的,研究结果发表在《国际科学转化医学》杂志上。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#乙肝新药#
25
#TRA#
32
#临床阶段#
33
#Med#
28
是很好的学习材料.不错.以后会多学习.
60