JACC:老年心衰患者植入左心室辅助装置(LVAD)后的临床预后
2021-09-02 Nebula MedSci原创
在老年心衰患者中,植入 LVAD 与活动能力、生活质量改善,以及并发症减少有关
根据我国最新流行病学调查显示,在我国≥35岁的居民中,心衰患病率约为1.3%,现约有1370万例心衰患者。随着年龄的增长,心衰的患病率明显升高,在65-79岁和80岁以上人群中,心衰的患病率分别高达3.85%和7.55%。老年心衰患者的一年死亡率高达20-30%。
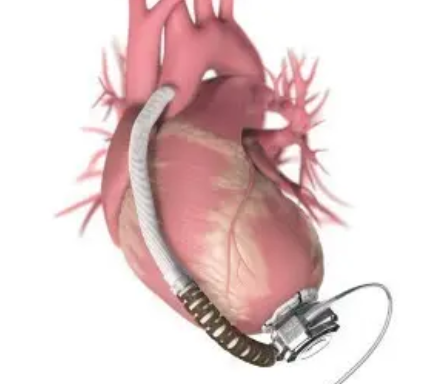
左心室辅助装置 (LVAD) 常用作4级心衰患者心脏移植的过渡治疗,或作为不适合移植的患者的终末治疗。但是,老年心衰患者植入 LVAD 后的生存率、功能结果和生活质量情况尚未完全明确,本研究旨在对此进行评估。
研究人员从INTERMACS 数据库中筛选了2010年1月1日至2020年3月1日期间植入持久性 LVAD 的成年患者。主要终点是校正生存率;次要终点包括使用视觉模拟量表评估的生活质量(0 表示最差,100 表示最好)、6 分钟步行距离、卒中、设备故障和再住院率。
该队列共包含16,808位(68.9%)65 岁以下的患者,6,418位(26.3%)65-75 岁的患者,1,182位(4.8%)75 岁以上的患者;大部分患者为男性(78%);一半以上的患者采用 LVAD 作为终末治疗(51%)。
65-75岁患者的死亡率
中位随访了15 个月。<65、65-75 和 >75 岁患者的死亡率分别是34%(70%CI 33-34%)、54%(54-55%)和66%(64-68%)。新一代 LVAD 设备与晚期死亡率降低有关(HR 0.35; 95%CI 0.25-0.49)。卒中、设备故障或血栓形成以及再住院率均随着年龄的增长而降低(所有p<0.01)。
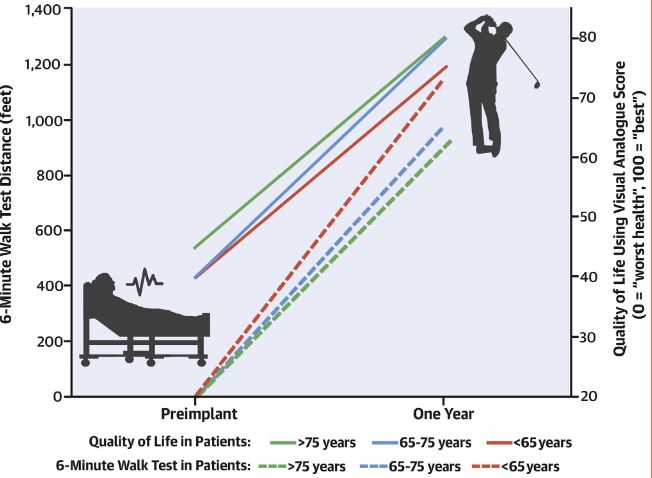
不同年龄段患者的生活质量和6分钟步行距离的变化
在所有年龄组中,植入 LVAD 后患者的中位6分钟步行距离从0步(范围 0-665步)增加到了1,065步(642-1,313步)(p<0.001),生活质量评分从 40 分增加到了 75 分(p<0.001)。
总而言之,在老年心衰患者中,植入 LVAD 与活动能力、生活质量改善,以及并发症减少有关;而且该相关性在年龄越大的患者中,越相对明显。
原始出处:
Emerson Dominic,Chikwe Joanna,Catarino Pedro et al. Contemporary Left Ventricular Assist Device Outcomes in an Aging Population: An STS INTERMACS Analysis.[J] .J Am Coll Cardiol, 2021, 78: 883-894.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#JACC#
0
#左心室辅助装置#
38
#心室辅助装置#
34
#ACC#
32
#心衰患者#
50
#左心室#
39
#植入#
29
#临床预后#
31
写的真好
55