Heart:STEMI患者:院前替罗非班治疗降低长期死亡率?
2017-09-27 安雅晶 环球医学
2017年10月,发表在《Heart》的一项由荷兰、意大利和德国科学家进行的安慰剂、对照、双盲、随机试验,考察了院前替罗非班治疗对ST段抬高心肌梗死(STEMI)患者长期死亡率的影响。
目的:研究人员进行了一项On-TIME2(心肌梗死使用替罗非班治疗评估2)的亚组分析,On-TIME2是一项安慰剂、对照、双盲、随机试验,旨在评估N末端B型钠尿肽(NT-proBNP)水平和长期(5年)死亡率之间的相关性,调查院前替罗非班给药对NT-proBNP水平相关死亡率的影响。
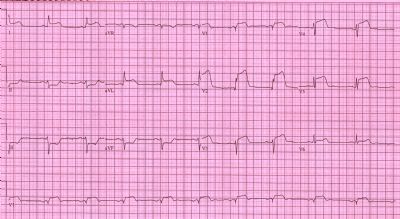
方法:总共984名正进行首次经皮冠状动脉介入治疗(PCI)的STEMI患者随机分配到救护车替罗非班或安慰剂治疗的组中。NT-proBNP水平在血管造影前住院(基线)和此后的18~96小时(PCI后)进行评估。
结果:918名(93.3%)患者的基线NT-proBNP值可评估,865名(87.9%)的PCI后值可评估。基线NT-proBNP水平高于中位值(137pg/mL)的患者比低于基线值的患者具有较高的30天(5.1% vs 0.2%,P<0.001)、1年(7.0% vs 0.7%,P<0.001)、5年(20.3% vs 4.9%,P<0.001)死亡率。多变量Cox分析显示,NT-proBNP高于中位值为5年死亡率的独立预测因素(HR,2.73;95% CI,1.47~5.06;P=0.002)。高于中位值且接受早期替罗非班治疗的患者比接受安慰剂治疗的患者具有显着性低的30天(2.7% vs 7.5%,P=0.021)和1年(4.5% vs 9.4%,P=0.043)死亡率。5年时,治疗组维持了较低但是非显着性的死亡率(18% vs 22.4%,P=0.265)。
结论:STEMI患者中,基线NT-proBNP水平可独立预测长期死亡率。基线NT-proBNP水平高于中位值的患者中,早期院前替罗非班治疗可显着降低30天和1年死亡率,表明高风险患者具有特别的获益。该结果应该在其他研究中予以证实。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#院前#
32
#STEMI患者#
57
#ART#
35
#STEM#
45
#HEART#
30
不错
64