Blood:CD19特异性CAR T细胞疗法治疗R/R B-ALL
2019-10-22 QQY MedSci原创
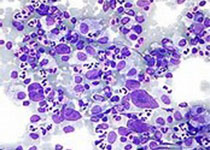
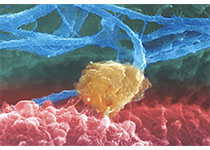
嵌合抗原受体(CAR) T细胞已被证明对复发性/难治性(R/R)B细胞急性淋巴细胞白血病(B-ALL)患者有临床效益。Curran等人开展一多中心的临床试验,研究CAR T细胞疗法的毒性、可行性和治疗反应性。共招募了25位R/R B-ALL儿科/年轻的成年患者(1-22.5岁),予以19-28z CAR T治疗。调节化疗包括高剂量(3g/m2)环磷酰胺(HD-Cy)和低剂量(≤1.5g/m2)环磷
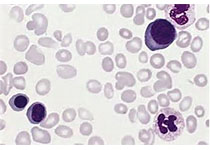
共招募了25位R/R B-ALL儿科/年轻的成年患者(1-22.5岁),予以19-28z CAR T治疗。调节化疗包括高剂量(3g/m2)环磷酰胺(HD-Cy)和低剂量(≤1.5g/m2)环磷酰胺(LD-Cy) ,相对应的患者分别是17位和8位。15位患者在治疗前存在微小残留病灶(MRD,<5%骨髓细胞),10位患者有治疗前的疾病形态学证据(≥5%骨髓细胞)。
所有的毒性反应都是可逆的,有重度CRS(16%,4/25)和重度神经毒性(28%,7/25)。接受治疗的患者均进行了反应评估,在可评估的患者中(24位), HD-Cy/MRD组的反应性和CAR T细胞扩增峰值均优于LD-Cy/形态学组,且无毒性增加。
本研究结果证明了CD19特异性CAR T细胞疗法可安全治疗R/R B-ALL,还提示调节化疗的剂量和治疗前的微小残留病灶负担均对治疗反应性有正性影响,且无增加毒性。
原始出处:
Kevin J. Curran, et al.Toxicity and Response following CD19-specific CAR T cells in pediatric/young adult relapsed/refractory B-ALL .Blood.2019001641. https://doi.org/10.1182/blood.2019001641
本文系梅斯医学(MedSci)原创编译,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#特异性#
34
#ALL#
26
#CD19#
42
#B-ALL#
40
#T细胞疗法#
38
学习了
71