[摘要] 乳腺癌较易发生脑转移,其发生率在恶性肿瘤中仅次于肺癌。三阴性乳腺癌(triple-negative breast cancer, TNBC)脑转移发生时间早、发生率高,且患者预后差。TNBC脑转移治疗的难点在于缺少靶向药物以及药物较难透过血脑屏障,以致全身治疗效果欠佳。目前包括手术和放疗在内的局部治疗仍是脑转移瘤的主要治疗手段,手术治疗能快速缓解脑转移患者的神经系统压迫症状,此外,手术联合放疗较单纯手术治疗或单纯放疗可改善脑转移患者预后。在放疗方面,全脑放疗(whole-brain radiation therapy,WBRT)是颅内多发转移、脑膜转移的标准治疗,WBRT可改善多发脑转移患者的生存情况,但会影响患者认知功能,要注意海马回的保护,因此对于有限数目脑转移的患者,脑部立体定向放疗已经取代全脑放疗。然而局部治疗难以有效地控制脑转移的进展且并发症较多,需辅以全身治疗等支持治疗。卡培他滨、顺铂等化疗药物可透过血脑屏障但其疗效有限,因此新型靶向药物的研发及新靶点的探索是TNBC脑转移研究的方向。近年来研究发现,携带BRCA基因突变的患者有更高的脑转移风险,脑转移患者BRCA突变比例亦较高。目前多腺苷二磷酸核糖聚合酶[poly(ADP-ribose)polymerase,PARP]抑制剂可用于晚期胚系BRCA1/2突变的TNBC患者,且可突破血脑屏障。Ⅲ期EMBRACA临床研究显示,PARP抑制剂talazoparib可使BRCA1/2突变的脑转移亚组获益。此外,抗体-药物偶联物(antibody-drug conjugate,ADC)德曲妥珠单抗也可透过血脑屏障,DEBBRAH等临床研究显示,德曲妥珠单抗在HER2阳性乳腺癌脑转移患者中疗效显著,在HER2低表达患者中研究目前还未达到终点,其在TNBC脑转移治疗中的效果令人期待。戈沙妥珠单抗为靶向TROP-2的新型ADC药物,Ⅲ期ASCENT临床研究显示在总体人群(包括脑转移患者)中戈沙妥珠单抗组与化疗组相比可显著延长晚期TNBC患者无进展生存期。肽-紫杉醇共轭物ANG1005已经在Ⅱ期临床研究中显示其对TNBC脑转移患者有疗效。另外,磷脂酰肌醇3-激酶(phosphoinositide3-kinase,PI3K)/蛋白激酶B(protein kinase,AKT) /哺乳动物雷帕霉素靶蛋白(mammalian target of rapamycin,mTOR)信号转导通路抑制剂、脂肪酸合酶抑制剂以及药物递迭系统等药物成为TNBC脑转移患者潜在的治疗方案。虽然Impassion 130研究结果显示,免疫治疗在TNBC脑转移无获益趋势,但基础研究显示放疗联合免疫治疗具有协同作用,目前有多项临床试验(NCT03483012、NCT03449238等)正在探索放疗与免疫治疗在乳腺癌脑转移中的疗效,结果令人期待。本文就TNBC脑转移治疗的研究进展进行综述。
[关键词] 三阴性乳腺癌;脑转移;局部治疗;化疗;靶向治疗;免疫治疗
[Abstract] Breast cancer has been the second most common solid tumor that metastasizes to the central nervous system after lung cancer. Triple-negative breast cancer (TNBC) has an earlier occurrence and high incidence of brain metastasis with its associated poor prognosis and limited treatment options due to the presence of the blood-brain barrier and lack of targeted drugs. Local treatment, including surgery and radiation therapy, are still the main therapy for brain metastasis. Surgical rep can not only relieve neurologic impairment of brain metastasis patients, but also can clarify the pathological type. Moreover, surgical rep combined with radiotherapy can improve the prognosis of brain metastasis patients compared to surgery or radiotherapy alone. By now, whole-brain radiation therapy (WBRT) is still considered the gold standard for multiple brain metastases, and meningeal metastases, but it will lead to neurocognitive decline, so hippocampal avoidance is essential. For selected patients with oligometastases, stereotactic radiotherapy has replaced WBRT to reduce cognitive toxicity. However, local treatment of TNBC brain metastasis cannot control the progress of brain metastasis and has significant side effects, so systemic therapy is needed. Chemotherapy drugs such as capecitabine and cisplatin can penetrate the blood–brain barrier, but their efficacy is limited. Therefore, the research and development of new targeted drugs and the exploration of new targets are necessary for TNBC brain metastasis. Research has found that patients carrying germline BRCA1/2 mutations have a higher risk of brain metastasis. Currently, the poly adenosine diphosphate ribose polymerase (PARP) inhibitor demonstrated antitumor activity in patients with advanced breast cancer and a germline BRCA1/2 mutation, and it can penetrate the blood-brain barrier. The phase Ⅲ trial EMBRACA reported that the PARP inhibitor talazoparib can prolong the progression-free survival of TNBC patients with brain metastasis. In addition, antibody drug conjugates (ADCs) trastuzumab deruxtecan (T-DXd) can also penetrate the blood-brain barrier. Studies such as DEBBRAH have shown that T-DXd has significant therapeutic effects in HER2 positive brain metastasis patients, while research on HER2 low expression patients has not yet reached the endpoint, and its role in TNBC brain metastasis is worth looking forward to. Sacituzumab govitecan (SG) is also an ADC composed of an antibody targeting the human trophoblast cell-surface antigen 2. The phase Ⅲ ASCENT study showed that in the full population (including 61 patients with brain metastasis), SG could significantly prolong the progression-free survival of advanced TNBC patients compared to the patients who received chemotherapy. ANG1005, a novel taxane derivative, can cross the blood–brain barrier as well. A multicenter, open-label phase Ⅱ study revealed that ANG1005 could prolong overall survival of patients with brain metastasis. In addition, phosphoinositide3-kinase, (PI3K)/protein kinase (AKT)/mammalian target of rapamycin (mTOR) pathway inhibitors, fatty acid synthase inhibitors, and the drugs with new delivery systems have become potential treatment options for TNBC brain metastasis patients. Although the Impassion 130 reported that no benefit trend for immunotherapy in TNBC brain metastasis, basic research has shown that radiotherapy combined with immunotherapy has a synergistic effect. Currently, multiple clinical trials (NCT03483012, NCT03449238, etc.) are exploring the efficacy of radiotherapy combined with immunotherapy in brain metastasis, and the results are promising. This article reviewed the research progress of TNBC brain metastasis treatment.
[Key words] Triple-negative breast cancer; Brain metastasis; Local therapy; Chemotherapy; Targeted therapy; Immunotherapy
乳腺癌是女性最常见的恶性肿瘤,是仅次于肺癌易发生脑转移的第二常见实体瘤,初诊时有5%的患者发生脑转移,进展中15%~30%的患者会发生脑转移[1]。其中三阴性乳腺癌(triple-negative breast cancer,TNBC)患者发生脑转移时间早、发生率高,在晚期TNBC中脑转移发生率为26%~46%[1-2]。TNBC是指雌激素受体(estrogen receptor,ER)、孕激素受体(progesterone receptor,PR)、人表皮生长因子受体2(human epidermal growth factor receptor type 2,HER2)表达均为阴性的乳腺癌,恶性程度高,患者预后差[2-3]。TNBC患者一旦发生脑转移则预后将非常差,生存期(overall survival,OS)一般短于6个月[2-3],且发生时往往伴随颅外转移瘤的进展[2]。由于血脑屏障的存在,许多化疗药物、靶向药物无法通过血脑屏障对脑内癌细胞进行杀伤[3-5],这也成为TNBC脑转移治疗的难点,目前TNBC脑转移仍以局部治疗为主[6-7]。
乳腺癌脑转移的治疗应采取多学科诊疗模式,治疗的目的是控制转移病灶,减轻患者症状,提高生活质量,最大限度地延长患者的生存时间[8-11]。治疗方式的选择取决于患者脑转移灶的位置、数目、大小、是否弥漫性转移、颅外疾病控制情况和卡式评分(Karnofsky Performance Status,KPS)等[8-11]。本文就TNBC脑转移治疗的研究进展进行综述。
1 局部治疗
由于血脑屏障的存在,TNBC脑转移全身治疗效果欠佳,截至目前,局部治疗仍是TNBC脑转移的主要治疗方式,包括外科手术治疗和局部放射治疗[12]。
1.1 外科手术
外科手术切除脑转移病灶能快速缓解患者的神经系统压迫症状,且能通过病理学检查明确肿瘤的病理学类型,是乳腺癌脑转移的有效治疗方法。有研究[13]结果显示,脑手术治疗后行全脑放射治疗(whole brain radiotherapy,WBRT)与单独WBRT治疗单发脑转移患者对比,接受手术后放疗的患者在原始转移部位复发的风险降低(20% vs 52%,P<0.02),中位OS更长(40周 vs 15周,P<0.01)。D’Andrea等[14]对71例接受手术治疗的脑转移患者进行回顾性研究。结果显示,术后无病情恶化,73.23%的患者神经检查病情显著改善(P<0.001),且患者实际OS是预期OS的2倍。此外,Goldberg等[15]对140例(其中乳腺癌脑转移占15%)术前KPS<70分且接受手术治疗的脑转移患者回顾性研究显示,患者中位OS为5.6个月,20%的患者术后KPS评分有显著改善(20 vs 40±20,P=0.048),且术后辅助放疗可以显著延长脑转移患者的OS(P=0.001)。该研究结果表明,手术治疗可以改善脑转移患者功能状态,也是部分低KPS患者适宜的治疗方式。
对于脑转移患者,脑手术治疗是安全可靠的,术后需联合放射治疗以改善患者生存情况。
1.2 放射治疗
放疗同样是乳腺癌脑转移局部治疗的重要手段。WBRT是脑转移的主要治疗方法,尤其是对于颅内多发性转移、弥漫性脑转移、脑膜转移的患者,行WBRT可显著延长患者的OS,行WBRT时需注意海马回保护[10,16]。由于WBRT会导致认知能力下降,因此对于有限数目脑转移患者,立体定向放射外科治疗(stereotactic radiosurgery,SRS)疗效值得进一步探索。
NCCTG N107C/CEC3研究[17]比较了脑转移术后行SRS和WBRT治疗的效果和安全性。结果显示,与接受WBRT的患者相比,SRS组无认知恶化OS更长[3.7个月 vs 3.0个月,风险比(hazard ratio,HR)=0.47,95% CI: 0.35~0.63,P<0.001]。6个月时认知恶化发生率也显著低于WBRT组(52% vs 85%,P<0.01),且两组患者的中位OS差异无统计学意义。但该研究并未针对TNBC脑转移人群开展, SRS对TNBC脑转移的有效性需进一步验证。
一项纳入68例(颅内转移灶≤5个)采用SRS治疗TNBC脑转移的多中心队列研究[18]结果显示,接受SRS治疗的TNBC脑转移患者1年OS率为43%,2年OS率为20%,此外,76%的病变显示退缩。该研究表明,SRS对经筛选的TNBC脑转移尤其是对那些具有良好表现状态且小至中等体积转移病灶的患者是安全有效的。
TNBC脑转移较非脑转移患者预后差[19]。对于有限数目脑转移的患者是否有必要在SRS基础上加做WBRT联合治疗?Medikonda等[19]对85例乳腺癌脑转移的患者进行回顾性队列分析研究,结果显示,入组的患者中TNBC占25%,其中52%的患者接受了WBRT,在接受WBRT患者中,82%的患者接受了SRS,64%的患者接受了手术治疗,Cox比例风险回归模型分析显示,WBRT对TNBC患者的OS无显著影响,可见对于有限数目脑转移的TNBC,在局部治疗的基础上加用WBRT并不能改善患者的OS。
接受TNBC脑转移局部治疗的患者的中位OS较短,因此在局部治疗控制的基础上,建议辅以全身药物治疗。此外,许多脑转移患者常伴颅外病灶进展,因此脑转移患者接受全身治疗对控制颅外病灶及维持中枢神经系统疾病的稳定和延长患者的OS具有重要意义。
2 全身治疗
2.1 化疗
化疗是TNBC的主要的治疗手段,Gao等[16]对277例TNBC脑转移患者进行评估,结果显示,接受化疗的患者比未接受化疗的患者中位OS延长6.6个月(9.0个月 vs 2.4个月)。但由于血脑屏障的存在,可用于TNBC脑转移的化疗药物较少,目前认为可透过血脑屏障的化疗药物包括卡培他滨、铂类药物等[7],但其疗效有限。
2.1.1 卡培他滨
卡培他滨是口服的抗代谢类药物,该药及其代谢产物可穿透血脑屏障,可以用于联合放疗或局部治疗后的维持治疗[7]。Gouveia等[20]回顾性分析了209例乳腺癌脑转移患者手术或放疗后应用卡培他滨单药治疗的效果,其中TNBC占26.4%,中位随访6个月,结果显示,TNBC脑转移中枢神经系统客观缓解率(objective response rate,ORR)较其他分子亚型高,但TNBC脑转移3个月的疾病控制率却较其他分子亚型低,中位无进展生存期(progression-free survival,PFS)仅为3.0个月,中位OS为4.5个月。此外,有研究[21]显示,TNBC脑转移应用卡培他滨联合放疗局部控制率会增加,但与仅接受放疗者相比患者的生存情况并未改善。总体而言,卡培他滨可用于TNBC脑转移维持治疗,但疗效有限。
2.1.2 顺铂
有研究[22]显示,顺铂联合吉西他滨治疗TNBC脑转移,中枢神经系统的ORR为66.6%,中位PFS为7.4个月(95% CI:2.4~12.3),但该研究TNBC脑转移仅6例。一项纳入113例乳腺癌脑转移患者(其中TNBC脑转移有15例)的Ⅱ期随机对照研究[23]探索了WBRT前行顺铂+依托泊苷+贝伐珠单抗全身治疗对比仅行WBRT组的脑特异性PFS。结果显示,WBRT前行化疗组较单纯WBRT组患者的中位脑特异性PFS显著延长(8.1个月 vs 6.5个月,HR=0.71;95% CI:0.44~1.13,P=0.15;显著性的预定义α≤0.20),且WBRT前行化疗组8个月脑特异性PFS率明显更高(48.7% vs 26.3%,P=0.03),因此含顺铂的联合治疗方案可以延长TNBC脑转移患者的PFS,提高局部控制率。
2.1.3 优替德隆
优替德隆(utidelone)是一种新型埃坡霉素类抗微管抑制药物,是非-P糖蛋白底物,美国食品药品管理局(Food and Drug Administration,FDA)已经批准优替德隆用于乳腺癌脑转移的患者。在2024年美国临床肿瘤学会(American Society of Clinical Oncology,ASCO)会议上,一项优替德隆联合贝伐珠单抗治疗HER2阴性乳腺癌脑转移的研究(NCT05357417)[24]显示,对于TNBC脑转移,中枢神经系统ORR为55%,中位PFS达8.4个月。研究证实,优替德隆对脑转移灶具有良好的抗肿瘤活性,为TNBC脑转移患者提供了新的治疗选择。
2.1.4 培戈-依诺替康(etirinotecan pegol,EP)
EP又名NKTR-102,是一种新型的长效的DNA拓扑异构酶Ⅰ抑制剂共轭聚合物类药物,可持续提供活性代谢物拓扑异构酶Ⅰ抑制剂SN-38[6]。临床前研究[25]显示,EP相比伊立替康可以提高TNBC脑转移模型的OS率。在 Ⅲ期BEACON研究[26]中,与医师选择的化疗(treatment of physician’s choice,TPC)相比, EP组乳腺癌脑转移患者的死亡风险显著降低(HR=0.51,P<0.01),中位OS分别为10.0和4.8个月,无论何种肿瘤亚型均有获益,其中TNBC亚型获益最明显(6.7个月 vs 3.8个月,HR=0.27)。但ATTAIN Ⅲ期研究[27]显示,在乳腺癌脑转移患者中,EP组和TPC组的中位PFS差异无统计学意义(3.9个月 vs 3.3个月,P=0.07),中位OS也相近(7.8个月 vs 7.5个月,P=0.60)。目前EP在TNBC脑转移中的疗效临床报道不一致,其在乳腺癌脑转移中应用还需要进一步的研究证实。
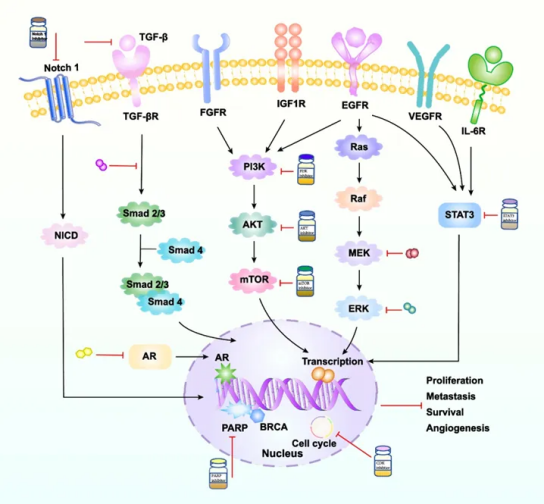
2.2 靶向治疗
由于ER、PR、HER2在TNBC表达均为阴性,缺乏内分泌治疗及抗HER2治疗的靶点。随着多腺苷二磷酸核糖聚合酶[poly(ADP-ribose) polymerase,PARP]抑制剂、抗体-药物偶联物(antibody-drug conjugate,ADC)等新型靶向药物的应用,为TNBC脑转移患者带来了新的希望。
2.2.1 PARP抑制剂
有研究[28]显示,携带BRCA基因突变的患者有更高的脑转移风险,脑转移患者BRCA突变比例亦较高。PARP抑制剂具有通过血脑屏障的优势,目前的一些指南[11,29]已经推荐晚期伴有胚系BRCA突变乳腺癌患者优先选择PARP抑制剂治疗,目前也有研究探讨其在伴有BRCA基因突变乳腺癌脑转移患者中的治疗价值。
维利帕尼(veliparib)是一种可以通过血脑屏障的口服PARP抑制剂。在一项veliparib联合WBRT治疗乳腺癌脑转移Ⅰ期临床试验[30]中,共纳入25例患者,6个月的OS率为61%(95% CI:39%~78%),颅内ORR为41%。一项顺铂加或不加veliparib治疗复发或转移性TNBC和(或)BRCA突变且伴有或不伴有脑转移的研究(NCT02595905)正在开展,结果值得期待。
艾尼帕利(iniparib)也是一种可以透过血脑屏障的PARP抑制剂。一项关于iniparib联合伊立替康治疗TNBC脑转移的有效性和安全性多中心、Ⅱ期临床试验[31]显示,iniparib联合伊立替康具有良好的耐受性,颅内病灶的反应率为12%,临床获益率为27%;颅外病灶的反应率为5%,临床获益率为11%。该研究证实iniparib联合伊立替康方案能够使TNBC脑转移患者获益。
他拉唑帕尼(talazoparib)是新一代的PARP抑制剂,有较强的催化阻滞活性。Talazoparib用于胚系BRCA1/2突变HER2阴性晚期乳腺癌。Ⅲ期EMBRACA临床研究[32]显示,与TPC组相比,talazoparib可显著改善患者的PFS和ORR;亚组分析中,脑转移亚组中PFS的获益甚至高于无脑转移患者(HR=0.32 vs HR=0.58)。但本研究没有进行颅内反应的评估。
2.2.2 ADC药物
德曲妥珠单抗(trastuzumab deruxtecan, T-DXd)是一种新型的ADC药物,具有更强的膜穿透性,可穿透至邻近细胞,避免与既往治疗出现交叉耐药,其拥有8∶1的药物抗体比,每个抗体可携带更多有效化疗药物[33]。DESTINY-Breas t01脑转移亚组分析[34]、DESTINY-Breast03研究[35]以及DEBBRAH研究[36]证实, T-DXd在治疗HER2阳性未经治、稳定性和活动性乳腺癌脑转移患者均显示出疗效,在HER2低表达的患者中的研究目前还未达到终点。这些研究均提示,T-DXd可以通过血脑屏障对颅内病灶进行杀伤。DESTINY-Breast04研究[37]证实,在HER2低表达转移性乳腺癌患者中,无论激素受体状态如何,T-DXd组的中位PFS(9.9个月 vs 5.1个月,HR=0.50,P<0.001)和OS(23.4个月 vs 16.8个月,HR=0.64,P=0.001)均显著长于TPC组,该研究中63例(11.3%)患者为TNBC。据统计,临床上45%~55%的HER2阴性患者应划分为HER2低表达,其中15.7%~53.6%为TNBC[38]。因此T-DXd能够为TNBC脑转移提供治疗选择但仍需大样本研究进行验证。
戈沙妥珠单抗(sacituzumab govitecan,SG)也是一种ADC药物,由靶向人滋养细胞表面抗原-2(Trop-2)的抗体通过可水解的连接子与DNA拓扑异构酶Ⅰ抑制剂SN-38偶联组成[39]。SG用于转移性TNBC的Ⅲ期ASCENT临床研究[39]共入组了61例稳定脑转移的患者,在总体人群中(伴或不伴脑转移的患者),与单药化疗相比,SG显著延长了患者的PFS(4.8个月 vs 1.7个月,HR=0.43,95% CI: 0.35~0.54, P<0.001),OS也较对照组延长了4.9个月(11.8个月 vs 6.9个月,HR=0.51,95% CI: 0.41~0.62)。此外,临床上有SG联合WBRT治疗伴BRCA突变的活动性脑转移的TNBC的成功报道[40],该患者SG联合放疗二线解救治疗能获得10个月的PFS,该结果为临床治疗TNBC脑转移指引了新的方向。此外,SHR-A1921是国内自主研发的针对Trop-2的抗体偶联物,其联合贝伐珠单抗在TNBC脑转移的前瞻性、单臂、单中心Ⅱ 期临床试验(NCT06210438)正在进行中。
2.2.3 ANG1005
ANG1005是一种新的肽-紫杉醇共轭物,由3个与angiopep-2共价结合的紫杉醇分子组成,可通过血脑屏障,并利用低密度脂蛋白受体相关蛋白1转运系统进入癌细胞[41]。一项关于ANG1005治疗乳腺癌脑转移的Ⅱ期临床研究[41]共入组72例患者,其中26%的患者为TNBC,研究显示,经ANG1005治疗的乳腺癌脑转移患者颅内和颅外临床获益率分别为77%和86%,乳腺癌脑转移患者的颅内总体ORR为15%,颅内临床获益率为68%。在TNBC中符合实体瘤疗效评价标准(Response Evaluation Criteria in Solid Tumors,RECIST)1.1版评估的13例患者中,有1例达到部分缓解,5例疾病稳定。该研究已经证实ANG1005对颅内转移病灶有杀伤作用,为TNBC脑转移药物治疗提供了新的选择。
2.2.4 PI3K/Akt/mTOR信号转导通路抑制剂
磷脂酰肌醇3-激酶(phosphoinositide3-kinase,PI3K)/蛋白激酶B(protein kinase,AKT)/哺乳动物雷帕霉素靶蛋白(mammalian target of rapamycin,mTOR)信号转导通路在43%~70%乳腺癌脑转移患者中发生改变,PI3K信号转导通路改变无关分子分型,该信号转导通路的激活可以促进肿瘤细胞的生长、增殖和血管生成等,成为乳腺癌脑转移治疗潜在的靶点[42-43]。GDC-0068[43]是一种选择性泛AKT抑制剂,体外研究显示与PIK3CA野生型细胞系相比,在PIK3CA突变的乳腺癌脑转移细胞系中,GDC-0068以剂量依赖性方式降低细胞活力,诱导细胞凋亡并抑制富含脯氨酸的AKT底物相对分子质量为40×103的p70 S6激酶的磷酸化。在PIK3CA突变的乳腺癌脑转移原位异种移植小鼠模型中,GDC-0068呈现有效的抗癌活性,然而其在临床中的应用有待相关临床试验进行验证。GDC-0084[44]是PI3K/mTOR双重抑制剂,具有血脑屏障通透性,目前相关临床试验主要在HER2阳性脑转移患者中开展(NCT03765983),其在TNBC脑转移中具有潜在的研究价值。
2.2.5 脂肪酸合酶(fatty acid synthase,FASN)抑制剂
有研究[45]发现脑转移的乳腺癌细胞相较于其他部位生长的肿瘤对脂肪酸合成的需求显著增高,与原发性乳腺癌活检相比,脑转移乳腺癌中FASN表达更高,抑制FASN能够有效地抑制乳腺癌细胞在颅内的生长。FASN抑制剂可以作为乳腺癌脑转移的潜在治疗策略。TVB-2640[46]是一种选择性FASN抑制剂,其与贝伐珠单抗联合用于星形细胞瘤的Ⅱ期临床试验结果显示,该方案的ORR达56%,其中完全缓解率为17%,部分缓解率39%,6个月PFS率为31.4%。FASN抑制剂在乳腺癌脑转移中的临床应用值得进一步探索。
2.3 免疫检查点抑制剂(immune checkpoint inhibitor,ICI)
一般情况下,健康的脑实质中没有淋巴细胞,属于免疫特权部位,但人类脑转移瘤已被证实有明显的T淋巴细胞浸润[7],且在脑转移瘤治疗中,尤其是黑色素瘤和非小细胞肺癌脑转移, ICI效果显著[31]。有研究[47]发现53%的乳腺癌脑转移患者表达程序性死亡配体-1(programmed death ligand-1,PD-L1),并且与分子分型无关,提示ICI在乳腺癌脑转移中有潜在的治疗作用。目前免疫治疗联合化疗可使局部晚期或转移性TNBC患者获益,FUTURE-C-Plus研究由复旦大学肿瘤医院邵志敏教授牵头,评估了在晚期免疫调节型TNBC中使用法米替尼(famitinib)联合卡瑞利珠单抗(camrelizumab)及白蛋白紫结合型紫杉醇的疗效及安全性,该研究也纳入了无症状的中枢神经系统转移的患者。结果显示,该方案治疗晚期免疫调节型TNBC疗效显著,安全性良好[48]。虽然Impassion 130研究[49]显示免疫治疗在TNBC脑转移中无获益趋势,但基础研究[50]显示放疗联合免疫治疗具有协同作用,可以减少肿瘤浸润髓源性抑制细胞的聚集,该细胞可抑制T淋巴细胞以及改变肿瘤免疫微环境。此外,放疗联合免疫治疗可激活细胞毒性T淋巴细胞产生肿瘤坏死因子来抑制肿瘤中髓源性抑制细胞的活性。目前有多项临床试验(NCT03483012、NCT03449238等)正在探索放疗与免疫治疗在乳腺癌脑转移中的效果,期待更多有关ICI与放疗或其他靶向药物治疗乳腺癌脑转移的临床研究结果问世。
2.4 其他靶点及治疗方法
有研究[51]发现,与原发乳腺肿瘤相比,组蛋白赖氨酸N-甲基转移酶2C(KMT2C)在远端转移中更常发生突变,KMT2C或KMT2D缺失通过KDM6A依赖的方式促进MMP3的表达,从而驱动TNBC的脑转移,为TNBC脑转移的治疗提供了新的靶点。Wu等[52]发现circKIF4A-miR-637-STAT3轴可促使TNBC脑转移,circKIF4A可以作为TNBC脑转移的预后生物标志物和治疗靶点。此外,为解决药物较难通过血脑屏障的问题,药物递迭系统的研究和开发显得尤为重要,如纳米颗粒药物递迭系统,其在TNBC中的应用正在不断探索中。另外,树突状细胞疫苗、嵌合抗原受体T淋巴细胞治疗等新型疗法成为TNBC脑转移潜在的治疗策略[7]。
3 展望
TNBC脑转移的治疗需要多学科参与,目前以外科手术和放射治疗为主,辅以全身系统治疗及对症支持治疗。由于血脑屏障存在,许多化疗药物无法进入颅内发挥疗效,卡培他滨及顺铂等传统化疗药物疗效有限,急需加快新的化疗药物以及靶向药物的研发以最终改善TNBC脑转移患者的预后。ADC药物、PARP抑制剂及免疫检查点抑制剂等药物的出现,为TNBC脑转移治疗带来了新的希望[53],但单药治疗效果欠佳,未来有望实现在局部治疗的基础上与更多治疗策略联合治疗,从而改善TNBC脑转移患者的预后。此外,PI3K信号转导通路抑制剂、FASN抑制剂以及药物递迭系统的研究成为TNBC脑转移潜在的治疗方案,随着新药的研发,未来TNBC脑转移的治疗效果将不断提高。
[参考文献]
[1] NIWINSKA A, POGODA K, JAGIELLO-GRUSZFELD A, et al. Intracranial response rate in patients with breast cancer brain metastases after systemic therapy[J]. Cancers, 2022, 14(4): 965.
[2] VENKITARAMAN R, JOSEPH T, DHADDA A, et al. Prognosis of patients with triple-negative breast cancer and brain metastasis[J]. Clin Oncol, 2009, 21(9): 729-730.
[3] IVANOVA M, PORTA F M, GIUGLIANO F, et al. Breast cancer with brain metastasis: molecular insights and clinical management[J]. Genes, 2023, 14(6): 1160.
[4] SUN H N, XU J N, DAI S, et al. Breast cancer brain metastasis: current evidence and future directions[J]. Cancer Med, 2023, 12(2): 1007-1024.
[5] BANSAL R, VAN SWEARINGEN A E D, ANDERS C K. Triple-negative breast cancer and brain metastases[J]. Clin Breast Cancer, 2023, 23(8): 825-831.
[6] SHAH N, MOHAMMAD A S, SARALKAR P, et al. Investigational chemotherapy and novel pharmacokinetic mechanisms for the treatment of breast cancer brain metastases[J]. Pharmacol Res, 2018, 132: 47-68.
[7] CHEN Q C, XIONG J, MA Y X, et al. Systemic treatments for breast cancer brain metastasis[J]. Front Oncol, 2023, 12: 1086821.
[8] VOGELBAUM M A, BROWN P D, MESSERSMITH H, et al. Treatment for brain metastases: ASCO-SNO-ASTRO guideline[J]. J Clin Oncol, 2022, 40(5): 492-516.
[9] 中国抗癌协会乳腺癌专业委员会, 中华医学会肿瘤学分会乳腺肿瘤学组. 中国抗癌协会乳腺癌诊治指南与规范(2024年版)[J]. 中国癌症杂志, 2023, 33(12): 1092-1187.
The Society of Breast Cancer China Anti-Cancer Association, Breast Oncology Group of the Oncology Branch of the Chinese Medical Association. Guidelines for breast cancer diagnosis and treatment by China Anti-cancer Association (2024 edition)[J]. China Oncol, 2023, 33(12): 1092-1187.
[10] 肖建平, 马玉超, 王 洁, 等. 中国肿瘤整合诊疗指南——脑转移瘤[J]. 癌症, 2023, 42(6): 304-318
XIAO J P, MA Y C, WANG J, et al. Chinese guidelines for integrated diagnosis and treatment of tumors-brain metastatic tumors[J]. Cancer, 2023, 42(6): 304-318
[11] 中国临床肿瘤学会指南工作委员会.中国临床肿瘤学会(CSCO)乳腺癌诊疗指南2024[M].人民卫生出版社,北京.
Organized by the Working Committee of the Guidelines of the Chinese Society of Clinical Oncology. Chinese Society of Clinical Oncology (CSCO) breast cancer diagnosis and treatment guide-2024[M]. Beijing: People’s Health Publishing House, 2024.
[12] GARSA A, JANG J K, BAXI S, et al. Radiation therapy for brain metastases: a systematic review[J]. Pract Radiat Oncol, 2021, 11(5): 354-365.
[13] PATCHELL R A, TIBBS P A, WALSH J W, et al. A randomized trial of surgery in the treatment of single metastases to the brain[J]. N Engl J Med, 1990, 322(8): 494-500.
[14] D’ANDREA G, PALOMBI L, MINNITI G, et al. Brain metastases: surgical treatment and overall survival[J]. World Neurosurg, 2017, 97: 169-177.
[15] GOLDBERG M, MONDRAGON-SOTO M G, ALTAWALBEH G, et al. Enhancing outcomes: neurosurgical rep in brain metastasis patients with poor Karnofsky performance score-a comprehensive survival analysis[J]. Front Oncol, 2024, 13: 1343500.
[16] GAO C, WANG F, SUKI D, et al. Effects of systemic therapy and local therapy on outcomes of 873 breast cancer patients with metastatic breast cancer to brain: MD Anderson Cancer Center experience[J]. Int J Cancer, 2021, 148(4): 961-970.
[17] BROWN P D, BALLMAN K V, CERHAN J H, et al. Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC·3): a multicentre, randomised, controlled, phase 3 trial[J]. Lancet Oncol, 2017, 18(8): 1049-1060.
[18] KOWALCHUK R O, NIRANJAN A, HESS J, et al. Stereotactic radiosurgery and local control of brain metastases from triple negative breast cancer[J]. J Neurosurg, 2023, 138(6): 1608-1614.
[19] MEDIKONDA R, SRIVASTAVA S, KIM T, et al. Development of new brain metastases in triple negative breast cancer[J]. J Neurooncol, 2021, 152(2): 333-338.
[20] GOUVEIA M C, HIDALGO FILHO C M, MORENO R A, et al. Activity of capecitabine for central nervous system metastases from breast cancer[J]. Ecancermedicalscience, 2023, 17: 1638.
[21] MILLS M N, NAZ A, THAWANI C, et al. Capecitabine and stereotactic radiation in the management of breast cancer brain metastases[J]. BMC Cancer, 2021, 21(1): 552.
[22] ERTEN C, DEMIR L, SOMALI I, et al. Cisplatin plus gemcitabine for treatment of breast cancer patients with brain metastases; a preferential option for triple negative patients?[J]. Asian Pac J Cancer Prev, 2013, 14(6): 3711-3717.
[23] CHEN T W, DAI M S, TSENG L M, et al. Whole-brain radiotherapy alone vs preceded by bevacizumab, etoposide, and cisplatin for untreated brain metastases from breast cancer: a randomized clinical trial[J]. JAMA Oncol, 2024, 10(3): 325-334.
[24] YAN M, LV H M, LIU X L, et al. Utidelone plus bevacizumab for the treatment of HER2-negative breast cancer brain metastases (U-BOMB): a multicenter, single-arm phase Ⅱ study[J]. J Clin Oncol, 2024, 42(16_suppl): 1081.
[25] ADKINS C E, NOUNOU M I, HYE T, et al. NKTR-102 Efficacy versus irinotecan in a mouse model of brain metastases of breast cancer[J]. BMC Cancer, 2015, 15: 685.
[26] CORTÉS J, RUGO H S, AWADA A, et al. Erratum to: prolonged survival in patients with breast cancer and a history of brain metastases: results of a preplanned subgroup analysis from the randomized phase Ⅲ BEACON trial[J]. Breast Cancer Res Treat, 2017, 166(1): 327-328.
[27] TRIPATHY D, TOLANEY S M, SEIDMAN A D, et al. Treatment with etirinotecan pegol for patients with metastatic breast cancer and brain metastases: final results from the phase 3 ATTAIN randomized clinical trial[J]. JAMA Oncol, 2022, 8(7): 1047-1052.
[28] RAGHAVENDRA A S, IBRAHIM N K. Breast cancer brain metastasis: a comprehensive review[J]. JCO Oncol Pract, 2024: OP2300794.
[29] GRADISHAR W J, MORAN M S, ABRAHAM J, et al. NCCN clinical practice guidelines in oncology breast carcinoma-V.4.2024[EB/OL]. National Comprehensive Cancer Network. Available at: http://www.NCCN.org.
[30] MEHTA M P, WANG D, WANG F, et al. Veliparib in combination with whole brain radiation therapy in patients with brain metastases: results of a phase 1 study[J]. J Neurooncol, 2015, 122(2): 409-417.
[31] MILLS M N, FIGURA N B, ARRINGTON J A, et al. Management of brain metastases in breast cancer: a review of current practices and emerging treatments[J]. Breast Cancer Res Treat, 2020, 180(2): 279-300.
[32] LITTON J K, RUGO H S, ETTL J, et al. Talazoparib in patients with advanced breast cancer and a germline BRCA mutation[J]. N Engl J Med, 2018, 379(8): 753-763.
[33] MODI S N, SAURA C, YAMASHITA T, et al. Trastuzumab deruxtecan in previously treated HER2-positive breast cancer[J]. N Engl J Med, 2020, 382(7): 610-621.
[34] JERUSALEM G, PARK Y H, YAMASHITA T, et al. Trastuzumab deruxtecan in HER2-positive metastatic breast cancer patients with brain metastases: a DESTINY-Breast01 subgroup analysis[J]. Cancer Discov, 2022, 12(12): 2754-2762.
[35] HURVITZ S A, HEGG R, CHUNG W P, et al. Trastuzumab deruxtecan versus trastuzumab emtansine in patients with HER2-positive metastatic breast cancer: updated results from DESTINY-Breast03, a randomised, open-label, phase 3 trial[J]. Lancet, 2023, 401(10371): 105-117.
[36] PÉREZ-GARCÍA J M, VAZ BATISTA M, CORTEZ P, et al. Trastuzumab deruxtecan in patients with central nervous system involvement from HER2-positive breast cancer: the DEBBRAH trial[J]. Neuro Oncol, 2023, 25(1): 157-166.
[37] MODI S N, JACOT W, YAMASHITA T, et al. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer[J]. N Engl J Med, 2022, 387(1): 9-20.
[38] ZHANG H N, PENG Y. Current biological, pathological and clinical landscape of HER2-low breast cancer[J]. Cancers, 2022, 15(1): 126.
[39] BARDIA A, HURVITZ S A, TOLANEY S M, et al. Sacituzumab govitecan in metastatic triple-negative breast cancer[J]. N Engl J Med, 2021, 384(16): 1529-1541.
[40] MAURO P D, SCHIVARDI G, PEDERSINI R, et al. Sacituzumab govitecan and radiotherapy in metastatic, triple negative, and BRCA-mutant breast cancer patient with active brain metastases: a case report[J]. Front Oncol, 2023, 13: 1139372.
[41] KUMTHEKAR P, TANG S C, BRENNER A J, et al. ANG1005, a brain-penetrating peptide-drug conjugate, shows activity in patients with breast cancer with leptomeningeal carcinomatosis and recurrent brain metastases[J]. Clin Cancer Res, 2020, 26(12): 2789-2799.
[42] ADAMO B , DEAL A M , BURROWS E , e t al. Phosphatidylinositol 3-kinase pathway activation in breast cancer brain metastases[J]. Breast Cancer Res, 2011, 13(6): R125.
[43] IPPEN F M, GROSCH J K, SUBRAMANIAN M, et al. Targeting the PI3K/Akt/mTOR pathway with the pan-Akt inhibitor GDC-0068 in PIK3CA-mutant breast cancer brain metastases[J]. Neuro Oncol, 2019, 21(11): 1401-1411.
[44] IPPEN F M, ALVAREZ-BRECKENRIDGE C A, KUTER B M, et al. The dual PI3K/mTOR pathway inhibitor GDC-0084 achieves antitumor activity in PIK3CA-mutant breast cancer brain metastases[J]. Clin Cancer Res, 2019, 25(11): 3374-3383.
[45] FERRARO G B, ALI A, LUENGO A, et al. Fatty acid synthesis is required for breast cancer brain metastasis[J]. Nat Cancer, 2021, 2(4): 414-428.
[46] KELLY W, DIAZ DUQUE A E, MICHALEK J, et al. Phase Ⅱ investigation of TVB-2640 (denifanstat) with bevacizumab in patients with first relapse high-grade astrocytoma[J]. Clin Cancer Res, 2023, 29(13): 2419-2425.
[47] DUCHNOWSKA R, PĘKSA R, RADECKA B, et al. Immune response in breast cancer brain metastases and their microenvironment: the role of the PD-1/PD-L axis[J]. Breast Cancer Res, 2016, 18(1): 43.
[48] 张 琪, 修秉虬, 吴 炅. 2023年中国乳腺癌重要临床研究成果及最新进展[J]. 中国癌症杂志, 2024, 34(2): 135-142.
ZHANG Q, XIU B Q, WU J. Progress of important clinical research of breast cancer in China in 2023[J]. China Oncol, 2024, 34(2): 135-142.
[49] SCHMID P, ADAMS S, RUGO H S, et al. Atezolizumab and nab-paclitaxel in advanced triple-negative breast cancer[J]. N Engl J Med, 2018, 379(22): 2108-2121.
[50] DENG L F, LIANG H, BURNETTE B, et al. Irradiation and anti-PD-L1 treatment synergistically promote antitumor immunity in mice[J]. J Clin Invest, 2014, 124(2): 687-695.
[51] SEEHAWER M, LI Z Q, NISHIDA J, et al. Loss of Kmt2c or Kmt2d drives brain metastasis via KDM6A-dependent upregulation of MMP3[J]. Nat Cell Biol, 2024, 26(7): 1165-1175.
[52] WU S, LU J B, ZHU H B, et al. A novel axis of circKIF4A miR-637-STAT3 promotes brain metastasis in triple-negative breast cancer[J]. Cancer Lett, 2024, 581: 216508.
[53] 张思源, 江泽飞. 2023年改变晚期乳腺癌临床实践的重要研究成果及进展[J]. 中国癌症杂志, 2024, 34(2): 143-150.
ZHANG S Y, JIANG Z F. Important research progress in clinical practice for advanced breast cancer in 2023[J]. China Oncol, 2024, 34(2): 143-150.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#三阴性乳腺癌# #脑转移# #免疫治疗# #局部治疗#
25