BJH:继发性髓外多发性骨髓瘤高危患者的识别
2021-12-12 MedSci原创 MedSci原创
具有未来 EMD 发展的 MM 患者显示出在 MM 诊断时已经存在的特定特征(年龄较小、广泛的骨病、IgA 或非分泌型 MM)
多发性骨髓瘤 (MM) 是第二常见的血液系统恶性肿瘤。它占所有癌症的 1.7% 和所有血液系统恶性肿瘤的 10%。过去的20年中,新颖的药物[蛋白酶抑制剂(PIs),免疫调节药物(各种IMiDs),单克隆抗体等已经显著延长存活(NDMM) 以及复发/难治性 MM (RRMM) 患者。更好的成像技术 [计算机断层扫描 (CT)、正电子发射断层扫描 (PET)、PET-CT 或磁共振成像 (MRI)] 显示出更高的所谓髓外骨髓瘤 (EMD) 检出率。然而,EMD 的原因尚未确定。
EMD分为原发性EMD(MM诊断时发现)和继发性EMD(MM复发时发现),继发性 EMD 的预后较差。根据不理想的治疗结果,临床需要尽早诊断出继发性EMD发展风险高的患者。不幸的是,在继发性 EMD 发生之前,缺乏关于患者临床特征的证据。因此,一研究团队在现实生活中的继发性 EMD 患者组中分析了 EMD 出现之前的病程。
他们在捷克共和国 2005 年至 2017 年间诊断出的 4 985 名 MM 患者中分析了 234 名继发性 EMD 患者,以阐明继发性 EMD 发展的危险因素。
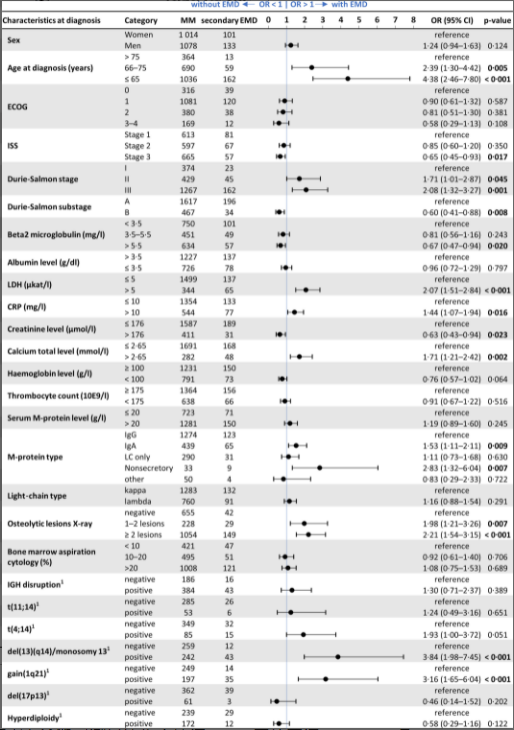
图1:多发性骨髓瘤 (MM) 和继发性髓外多发性骨髓瘤 (EMD) 患者在诊断时测量的临床特征。CI,置信区间;CRP,C-反应蛋白;ECOG,东部肿瘤合作组;IGH,免疫球蛋白重链;ISS,国际分期系统;LDH,乳酸脱氢酶;或者,总体反应。
他们发现年龄较小 [<65 岁;优势比 (OR) 4·38,95% 置信区间 (CI):2·46–7·80,P < 0·0001],高乳酸脱氢酶 (LDH) 水平 (>5 μkat/l;OR 2·07 , 95% CI: 1·51-2·84, P < 0·0001), 广泛的溶骨活性 (OR 2·21, 95% CI: 1·54-3·15, P < 0·001), 和免疫球蛋白A(IgA;OR 1·53,95% CI:1·11–2·11,P = 0·009) 或非分泌型 MM (OR 2·83; 95% CI: 1·32–6·04, P = 0·007) 是 MM 诊断时的主要危险因素二次 EMD 开发。

图2:未来继发性髓外多发性骨髓瘤 (EMD) 发展对不同治疗线中无进展 (PFS) 和总体 (OS) 生存率的影响。CI,置信区间;NDMM,新诊断的多发性骨髓瘤;RRMM,作为复发/难治性多发性骨髓瘤。
与没有未来 EMD 的 NDMM 患者相比,新诊断的 MM (NDMM) 患者有后续 EMD 的中位无进展 (PFS) 和总 (OS) 生存率较低 [mPFS:13·8 个月(95% CI:11·4-16) ·3) 对比 18·8 个月(95% CI:17·7–19·9),P = 0·006;mOS:26·7 个月(95% CI:18·1-35·4)与 58·7 个月(95% CI:54·8-62·6),P < 0·001]。
总的来说,他们发现具有未来 EMD 发展的 MM 患者显示出在 MM 诊断时已经存在的特定特征(年龄较小、广泛的骨病、IgA 或非分泌型 MM)。在 NDMM 患者中,在 MM 诊断后不久发生继发性 EMD,从一开始就显示出侵袭性的疾病模式。在更多预先治疗的 MM 患者中,继发性 EMD 发展之前的病程与其他 MM 患者相似。在未知事件之后,EMD 可能作为 MM 进化中的一个终端事件发生。无论何时,当 PCs 失去对 BM 微环境的依赖时,病程发生绝对周转,导致过早死亡。也证实了继发性 EMD 发展是 MM 的一个强大的独立负面预后因素。
原始出处:
Stork M, Sevcikova S, Minarik J, Krhovska P, Radocha J, Pospisilova L, Brozova L, Jarkovsky J, Spicka I, Straub J, Pavlicek P, Jungova A, Jelinek T, Sandecka V, Maisnar V, Hajek R, Pour L. Identification of patients at high risk of secondary extramedullary multiple myeloma development. Br J Haematol. 2021 Nov 2. doi: 10.1111/bjh.17925. Epub ahead of print. PMID: 34726261.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#高危患者#
38
#继发性#
44
#继发#
52
#多发性#
34
学习了
46
学习了
55