JAHA:晚期肾病的心肌细胞骨架适应性变化
2022-02-18 MedSci原创 MedSci原创
晚期慢性肾病的心肌衰竭特征是细胞骨架受损,包括粘着斑通路的破坏、线粒体衰竭和细胞存活通路的丧失。
心脏衰竭是慢性肾脏病(CKD)患者死亡的主要原因。在CKD病程早期发生心脏不良改变,包括左心室肥大(LVH)、左心室扩张、心肌纤维化和钙化,导致左心室舒张功能障碍比收缩功能障碍更常见。这些改变被描述为与CKD相关的心肌病,部分归因于容量超负荷、电解质紊乱和循坏毒素累积。此外,慢性血液透析会导致LV节段性心肌休克和冬眠,从而促进心肌适应性进展。心肌细胞骨架是细胞器功能、生物能量代谢和心肌重塑的关键基础。迄今为止,伴有晚期慢性肾病的心衰患者心肌细胞骨架损伤的发生情况在很大程度上尚未明确。

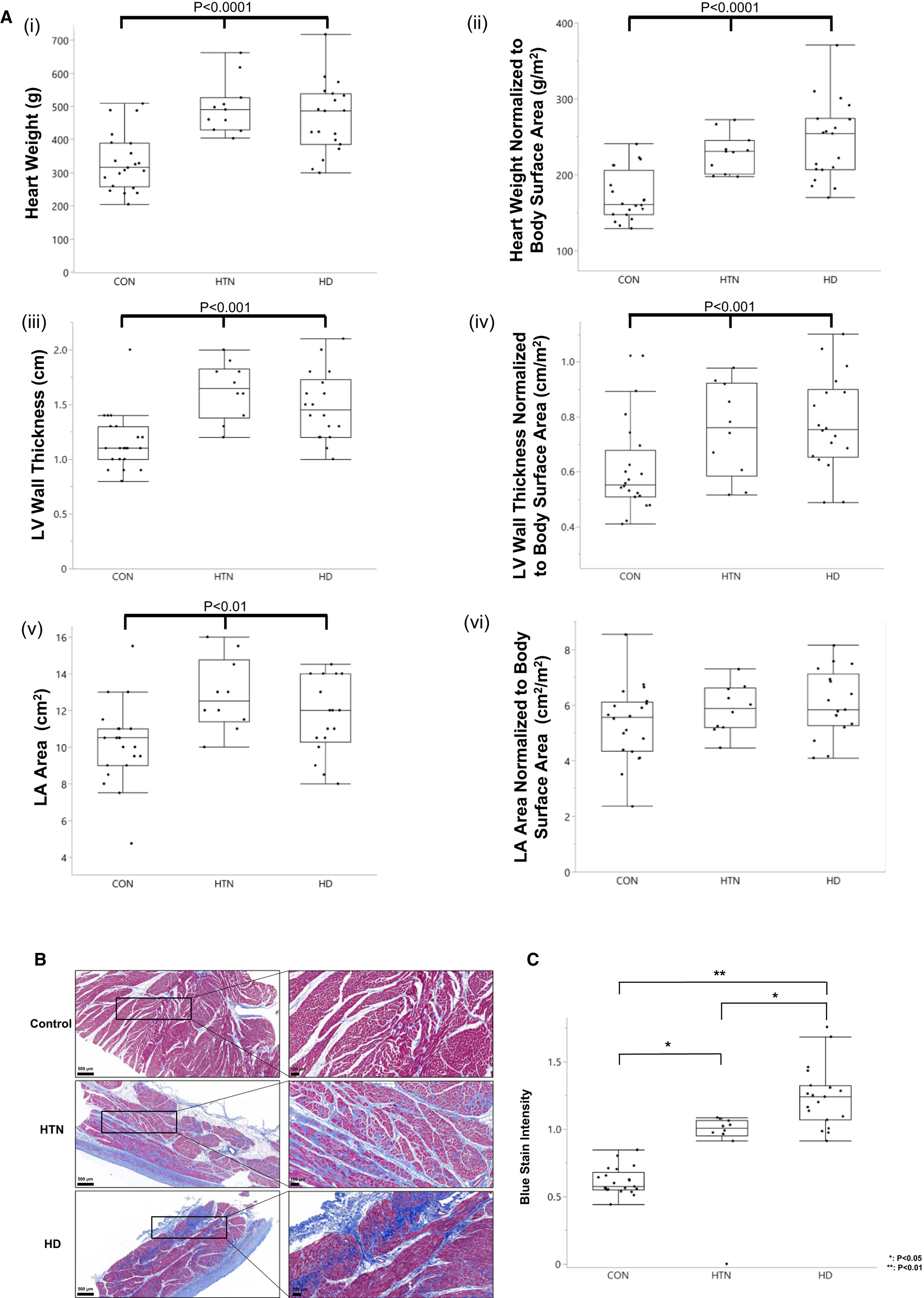
近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员对来自依赖血液透析的患者(n=19)、肾功能正常的高血压患者(n=10)和健康对照组(n=21)的移植人体心脏组织进行了一项3组的横断面队列研究。研究人员对左心室组织进行了病理学检查和新一代RNA测序。利用体外人心脏成纤维细胞模型进行了分子机制和干扰RNA研究。
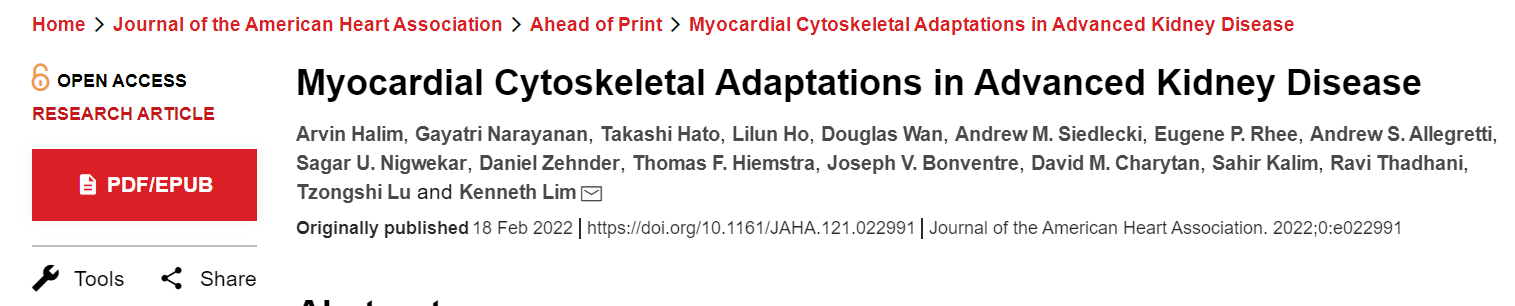
与高血压患者(P<0.05)和对照组(P<0.01)相比,血液透析患者的左心室组织心肌壁厚度增加,纤维化程度显著增加。转录组学分析显示,在接受血液透析的患者的心脏中,粘着斑通路显著富集。接受血液透析的患者心脏表现出粘着斑通路的失调,包括与对照相比,β-肌动蛋白(P<0.01)、β-微管蛋白(P<0.01)和波形蛋白(P<0.05)表达减少,以及纽蛋白表达增加(P<0.05)。
血液透析组心脏的细胞骨架适应与线粒体生物能量学受损相关,包括线粒体动力学和融合失调,以及细胞存活途径的丧失。机制研究表明,细胞骨架的变化可以由体外慢性肾病的尿毒症和代谢异常所导致。此外,通过干扰RNA进行的粘着斑激酶沉默与体外慢性肾病中发现的电解质应激协同抑制主要细胞骨架蛋白。
由此可见,晚期慢性肾病的心肌衰竭特征是细胞骨架受损,包括粘着斑通路的破坏、线粒体衰竭和细胞存活通路的丧失。
原始出处:
Arvin Halim.et al.Myocardial Cytoskeletal Adaptations in Advanced Kidney Disease.JAHA.2022.https://www.ahajournals.org/doi/10.1161/JAHA.121.022991
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#晚期肾病#
38
#AHA#
31
#适应性#
41
学习
42