中国研究成果“IBI303”登上《柳叶刀·风湿病学》封面
2019-09-03 张素 中国新闻网
由清华大学临床医学院教授徐沪济牵头、针对国产生物类似药大型临床Ⅲ期研究成果刊登在近日出版的子刊《柳叶刀·风湿病学》,并获封面推介。
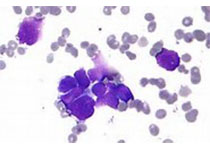
强直性脊柱炎(AS):“不死的癌症”
强直性脊柱炎是一种慢性炎症性疾病,主要侵犯骶髂关节、脊柱骨突、脊柱旁软组织及外周关节,也可累及关节外器官,如眼、皮肤以及心血管系统。它具有高致残率和高复发率,被称为“不死的癌症”。5%的患者在确诊1年后即丧失劳动力,45%的患者在起病10年内会出现严重的关节功能障碍,30%以上的患者20年后完全不能工作。
“AS主要侵害18至40岁青壮年男性,中国至少有500万青壮年男性罹患AS,而且青壮年患者常因病痛无法正常工作和生活,致使其容易出现心理和生理障碍。”徐沪济说。
目前,中国对AS患者的标准治疗方案是非甾体类抗炎药、缓解病情抗风湿药、糖皮质激素以及生物制剂等。其中肿瘤坏死因子α抑制剂具有良好的抗炎和阻止疾病进展的作用,是目前国内外AS治疗中,使用最为广泛、临床研究支持数据最多的生物制剂。
IBI303:信达生物自主研发比肩原研药
此次获得刊登的研究,是在活动性强直性脊柱炎患者中开展的比较IBI303(信达生物自主开发的重组人抗肿瘤坏死因子—α单克隆抗体注射液)和原研药阿达木单抗(商品名:修美乐)的疗效和安全性的多中心、随机、双盲、平行对照Ⅲ期临床研究,是国际上首次公开发表的关于阿达木单抗生物类似药和原研药在活动性强直性脊柱炎患者中的大型头对头Ⅲ期临床研究。
徐沪济团队负责的这项多中心、随机、双盲的原研药平行对照Ⅲ期研究,共有20家国内的医学中心参与。受试者是18周岁以上,非甾体抗炎药治疗4周以上疗效不佳、无效或无法耐受的活动性强直性脊柱炎患者。
结果表明,信达生物自主研发的阿达木单抗生物类似药IBI303,在治疗强直性脊柱炎的疗效、安全性上可比肩国外原研药。“这一研究结果被《柳叶刀·风湿病学》杂志接受,表明了信达生物在生物类似药领域从工艺开发到临床研发均达到了国际先进水准,同时也代表中国临床研究水平和研究者的能力与素质比肩国际水平。”徐沪济说。
研发团队:推动生物类似药造福患者
可用于治疗AS的修美乐(阿达木单抗)是全球第一个上市的全人源化抗TNF—α药物,2018年的销售额达到199亿美元。但修美乐在中国的市场只维持在不到1%的份额,主要原因是原研药价格高且缺少医保覆盖。
记者了解到,生物类似药和化学仿制药都属于仿制药类别,但研发生物类似药所需的时间和资金成本都远高于化学仿制药。原国家食药监总局在2015年发布了《生物类似药研发与评价技术指导原则(试行)》,极大地促进了本土生物类似药的研发。
信达生物制药董事长兼总裁俞德超表示:“强直性脊柱炎等自身免疫性疾病虽不致命,但是如果治疗不及时规范,将严重影响患者的生活质量。希望通过大家的努力,推动高质量的生物药早日上市,让更多的患者及其家庭从中受益。”
国际顶级风湿病学专家、美国德克萨斯大学西南医学中心教授斯坦利·科恩(Stanley Cohen)也在《柳叶刀·风湿病学》撰写评述称:“生物类似药在一些国家带来的大幅度费用下降,我们希望在中国也能变成现实。”
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#IBI303#
37
#研究成果#
31
AS:不死的癌症”
72
AS:不死的癌症
65
AS的治疗任重道远!
71