第十七届中国介入心脏病学大会(CIT2019)|陈韵岱:心肌微循环灌注的评价方法
2019-03-31 Gill MedSci原创
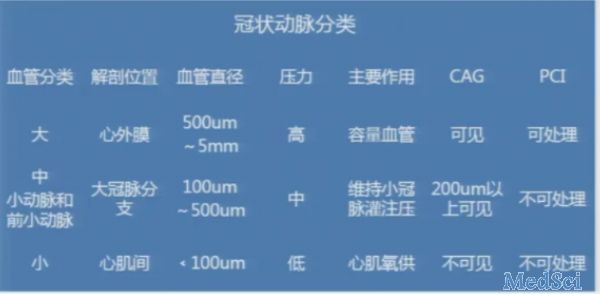
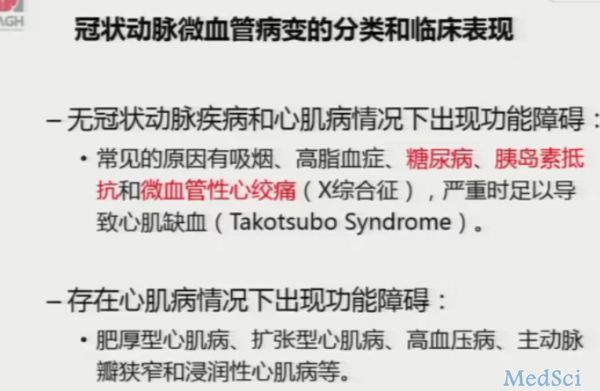
第十七届中国介入心脏病学大会(CIT2019)目前正在北京国家会议中心火热进行中,本次大会云集国内外心脏介入治疗专家泰斗,其中来自解放军总医院心内科的陈韵岱主任,对心肌微循环灌注的评价方法进行了专题讲座。冠状动脉分类微循环是指直径小于150um的微动脉和微静脉之间的血液循环,微动脉管壁含有平滑肌细胞,在交感、副交感神经和体液因子参与和调节下产生舒张和收缩活动,可引起相应的血管腔直径改变。冠状动脉微
第十七届中国介入心脏病学大会(CIT2019)目前正在北京国家会议中心火热进行中,本次大会云集国内外心脏介入治疗专家泰斗,其中来自解放军总医院心内科的陈韵岱主任,对心肌微循环灌注的评价方法进行了专题讲座。
冠状动脉分类
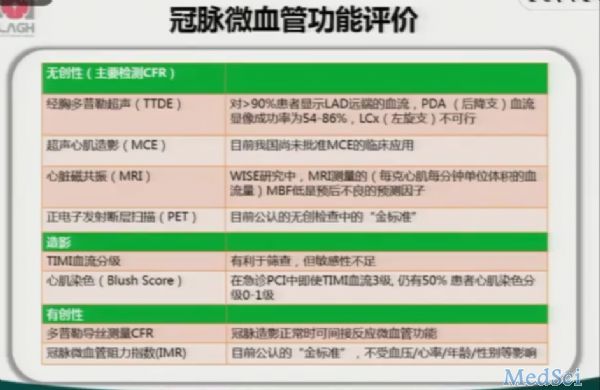
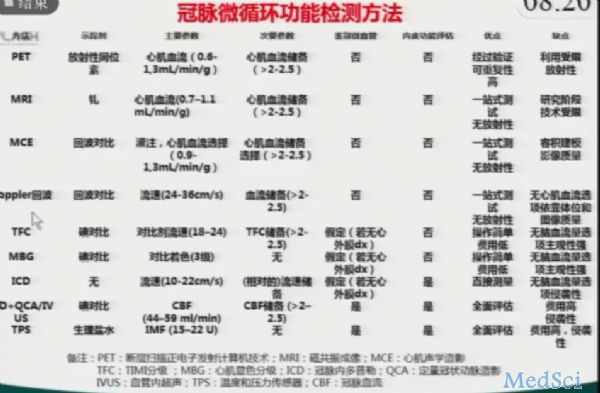
冠脉微血管功能评价的方法主要包括:
各种冠脉微循环检测方法具有各自的优缺点,应根据不同的阶段和需求选择合适的方法。
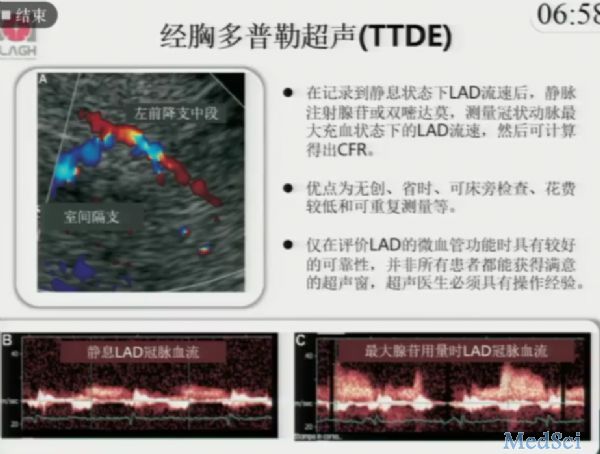
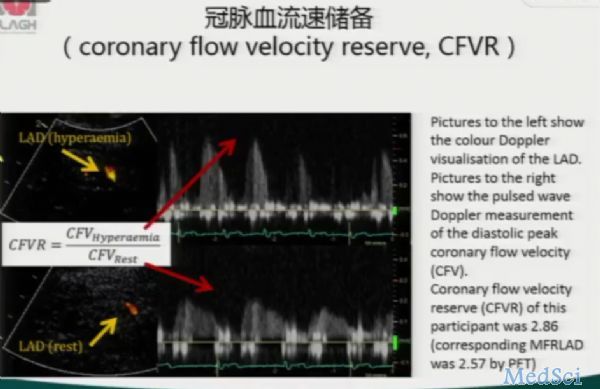
经胸多普勒超声(TTDE)是无创有效的一种检测方法。
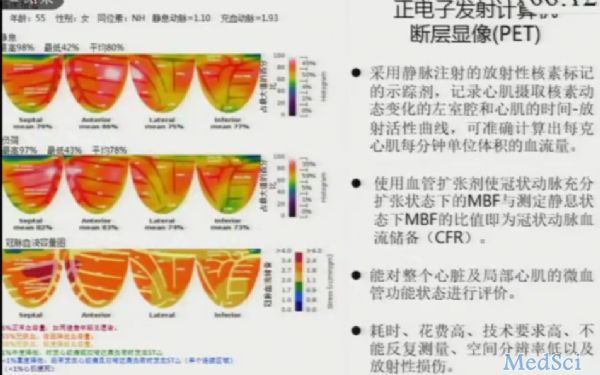
PET则需要借助于放射性同位素,可对整个心脏及局部心肌的微血管状态进行评价。但其存在耗时、花费高、重复差以及放射性损伤等缺点。
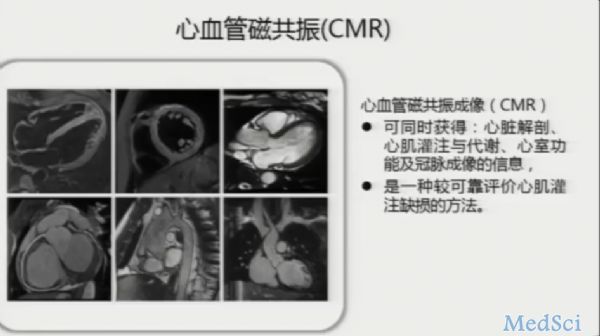
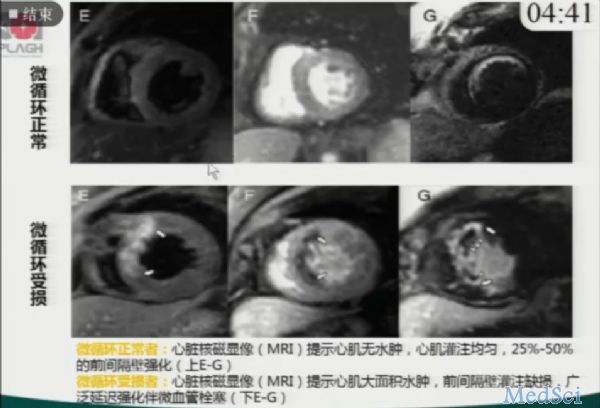
心血管磁共振是比较可靠的评价心肌灌注缺损的方法,并且与PET具有良好的相关性,但目前全国范围内CMR开展较少。
冠脉血流储备(CFVR)指冠状动脉在需求增加时能增加血流的能力,若降低则提示心肌缺血或冠状动脉微循环损害。
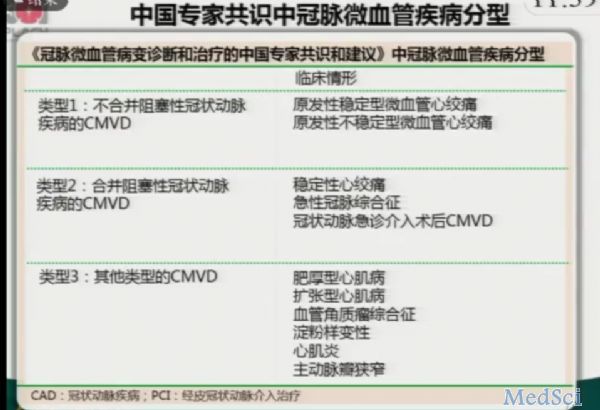
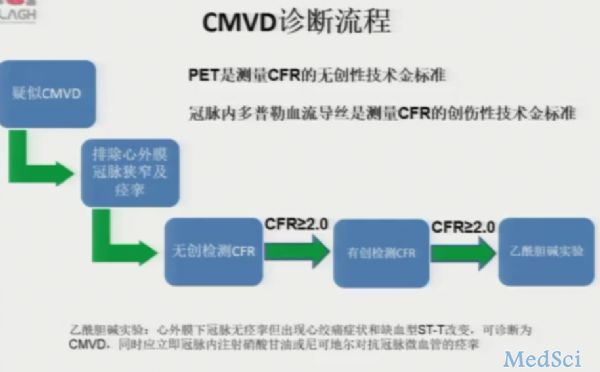
冠脉微血管疾病(CMVD)诊断流程:
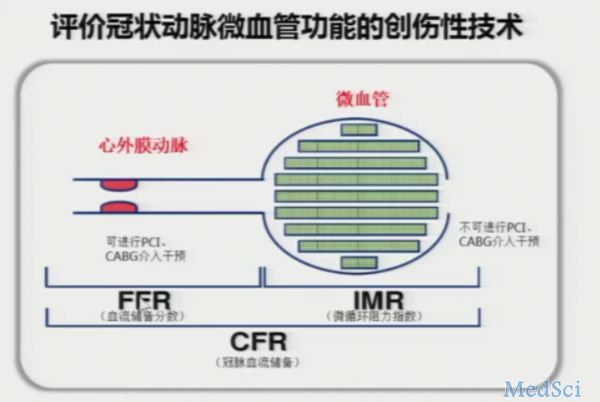
评价冠脉微血管功能的有创性技术
冠脉血流储备包括血流储备分数(FFR)、冠脉血流储备(CFR)、微循环阻力指数(IMR)。
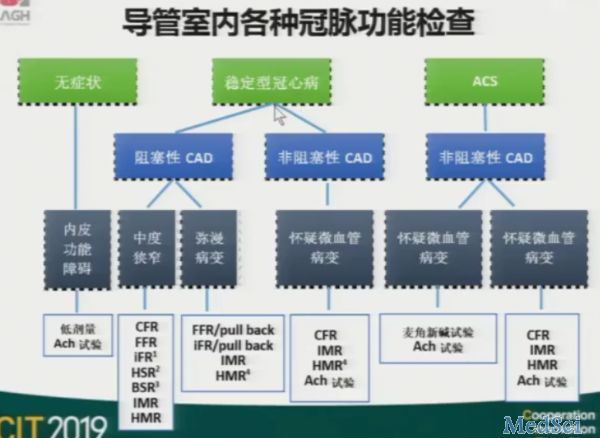
导管室内具备各种冠脉功能检查的方法,首先应对冠脉临床表型进行分类,结合内皮功能障碍、中度狭窄和弥漫性病变再就选择检测手段。
各类冠脉功能评估指标具有各自的定义和优缺点。
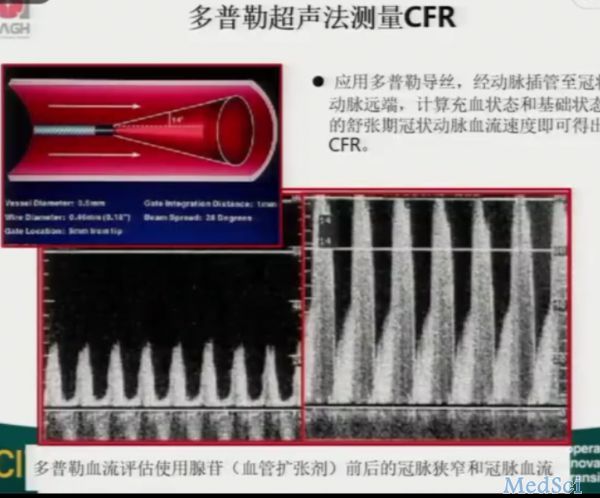
多普勒超声法测量CFR:
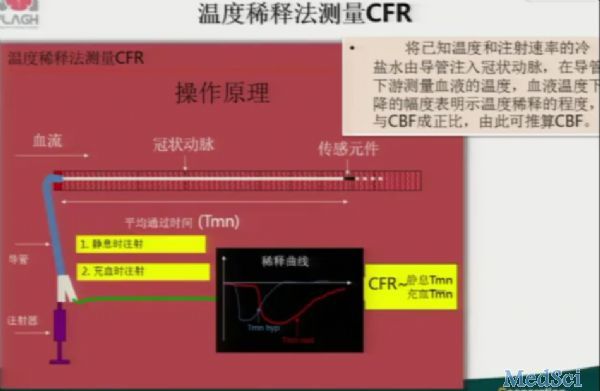
温度稀释法测量CFR:
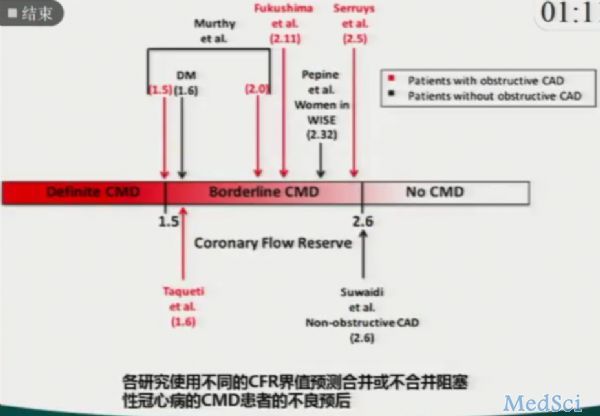
各研究使用不同的CFR界值预测CMD患者预后,总体上看,当CFR>2.0时,预后较良好。
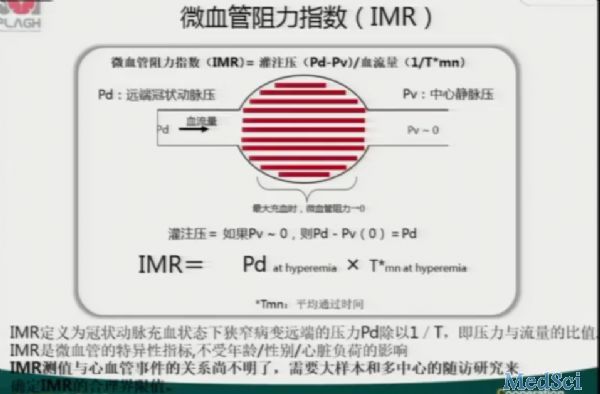
微血管阻力指数(IMR)定义为冠状动脉充血状态下狭窄病变远端的压力Pd除以1/T,即压力与流量的比值。
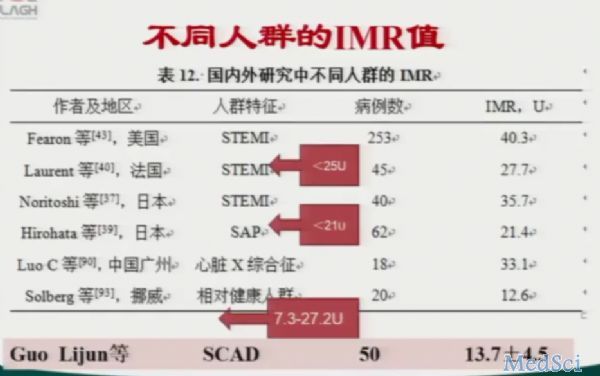
IMR是目前冠脉微血管功能障碍的最佳指标,重复性好,不受血流动力学影响。目前,尚无公认IMR正常值或者诊断切点。综合文献,目前不同研究使用切点总结如下表:
不同人群的IMR值具有差异:
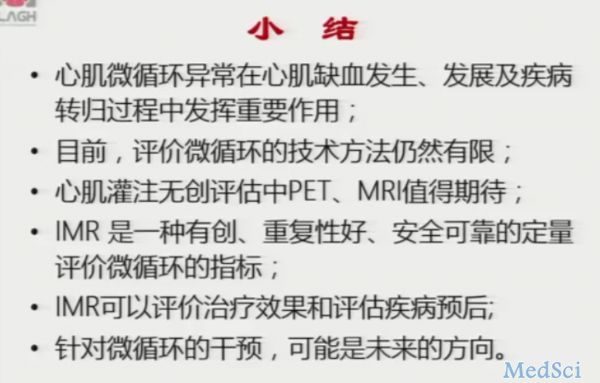
目前已经进入冠脉微循环时代,但目前仍存在诸多疑问和局限,有待进一步突破和解释。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#介入心脏病学#
37
#心脏病学#
35
#微循环#
45
#CIT#
29
#评价#
33