Ann Oncol:ER阳性患者的更佳cut-off值:1% vs. 10%?
2017-08-04 肿瘤资讯编辑部 肿瘤资讯
目前,将ER或PR表达<1%的患者定义为HR阴性肿瘤,但ER表达1-9%是否能从辅助内分泌治疗中获益,临床上尚存争议。近期,一项来自MD安德森肿瘤中心的回顾性分析提示,ER表达≥1%且<10%的患者可能与ER表达≤1%的患者有相似的分子特征和临床预后。
目前,将ER或PR表达<1%的患者定义为HR阴性肿瘤,但ER表达1-9%是否能从辅助内分泌治疗中获益,临床上尚存争议。近期,一项来自MD安德森肿瘤中心的回顾性分析提示,ER表达≥1%且<10%的患者可能与ER表达≤1%的患者有相似的分子特征和临床预后。
背景
根据美国临床肿瘤学会/美国病理学会(ASCO/CAP)的定义,ER或PR表达<1%的患者定义为HR阴性肿瘤。但既往的回顾性研究提示,ER表达1-9%的乳腺癌患者与ER<1%的患者基因表达谱相似。另一个回顾性研究同时纳入了HER2阳性和HER2阴性肿瘤,结果显示,ER表达1-9%和ER表达<1%的患者无复发生存期(RFS)和总生存期(OS)无统计学差异(分别为P=0.96和P=0.10),且两组患者的RFS和OS均显着劣于ER≥10%的患者。以上研究结果提示,ER表达≥1%且<10%的患者与ER表达≤1%的患者有相似的分子特征和临床预后。另一个回顾性研究提示,ER低表达的患者,以ER表达作为连续性变量,与更高的pCR率相关。然而,以上研究并没有区分HER2阳性和HER2阴性患者。此外,既往的研究都没有根据pCR率或从辅助内分泌治疗的生存获益上来探索ER表达阳性的最佳cut-off值。一些研究报道了HR阳性的患者对化疗的敏感性不如HR阴性的患者,这就提示,ER表达水平与新辅助化疗的敏感性相关。近期,St. Gallen国际专家共识2015指出,ER表达在1-9%的患者是否为ER阳性患者是存在争议的,这部分患者不能仅接受内分泌治疗。
目前,对于HER2阴性的患者,若将ER表达的百分比看作连续型变量,是否影响新辅助化疗的pCR率呢?能否根据患者从辅助内分泌治疗的获益多少,对三阴性乳腺癌来进行新的临床定义呢?目前,尚未可知。在本研究中,作者假设,HER2阴性的原发性乳腺癌,以ER表达率10%作为ER阳性的cut-off值相比1%能更好的区分,从新辅助化疗中取得更高pCR率的患者和能从辅助内分泌治疗中获得长期获益的患者。这一回顾性研究的主要目的是在II-III期HER2阴性的,原发性乳腺癌中,发现能从新辅助化疗的取得pCR的ER表达界值;此外,评估这一cut-off值能不能区分患者从辅助内分泌治疗中获益。
方法和结果
本研究纳入了MD安德森癌症中心1982-2013年间,II-III期HER2阴性的原发性浸润性乳腺癌患者,患者接受了新辅助化疗之后行根治性手术,且患者的ER和PR表达水平可知。共纳入3055例患者,其中II期和III期的患者分别占1726例(56.5%)和1329例(43.5%)。ER<1%,≥1%且<10%,≥10%的患者分别有932例(30.5%),171例(5.6%)和1952例(63.9%)。大多数的患者(2651例;86.8%)接受A+T的新辅助化疗。171例ER≥1%且<10%的患者中,43例(25.1%)接受了辅助内分泌治疗;1952例ER≥10%的患者中,1906例(97.6%)接受了辅助内分泌治疗。
在单因素logistic回归分析中,将ER和PR表达百分比看作连续型变量,ER和PR高表达与新辅助化疗更低的pCR率有关(ER:OR 0.98;95%CI:0.978-0.983;P<0.001;PR:OR 0.976;95%CI:0.971-0.98;P<0.001)。与这一结果一致,将ER和PR低表达作为分类变量,与新辅助化疗显着更高的pCR率有关。导管癌,临床分期II期,更高的核分级,A+T方案与显着更高的pCR率有关。
在多因素logistic回归分析中,将ER和PR表达百分比看作连续型变量,在调整了其他变量后,ER和PR低表达仍与新辅助化疗更高的pCR率有关(ER:OR 0.99;95%CI:0.986-0.994;P<0.001;PR:OR 0.989;95%CI:0.984-0.995;P<0.001)。导管癌,临床分期II期,更高的核分级,A+T方案仍与显着更高的pCR率有关。当根据ER的表达水平进行分组,与ER≥10%的患者相比,ER<1%或1%≤ER<10%的患者有显着更高的pCR率(ER<1%:OR,2.15;95%CI,1.62-2.87;P<0.001;1%≤ER<10%:OR,2.27;95%CI,1.48-3.47;P<0.001)。在多变量分析中,ER<1%和1%≤ER<10%组患者的pCR率没有统计学差异。
采用决策树模型,纳入3055例患者,根据pCR率来探寻ER阳性的最佳cut-off值,结果显示ER表达9.5%可推荐作为预测患者能否从新辅助化疗中取得pCR的截断值。多变量分析显示,ER<10%的患者对比ER≥10%的患者,pCR率显着更高,分别为26.6% vs. 7.0%(OR,2.17;95%CI,1.64-2.87;P<0.0001)。以此相同的方法来分析患者TTR的ER表达cut-off值,也为9.5%。
中位随访时间3.9年,ER<1%和1%≤ER<10%组患者的TTR和OS曲线交叉,但ER≥10%的患者,TTR和OS率显着高于ER<1%或1%≤ER<10%组患者(TTR和OS的P值均<0.0001),见下图1A和1B。当以10%作为ER表达阳性的cut-off值时,ER<10%的患者,TTR和OS均显着低于ER≥10%的患者(TTR和OS的P值均<0.0001),见下图1C和1D。而ER<1%和1%≤ER<10%组患者的的TTR或OS都没有显着统计学差异。
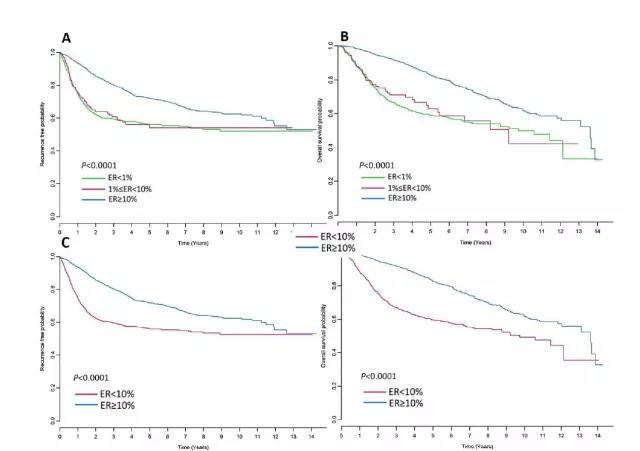
图1. TTR和OS分析. A,B: ER<1%组、1%≤ER<10%组和ER≥10%组患者的TTR和OS曲线。C,D:ER<10%和ER≥10%组患者的TTR和OS曲线对比。
研究者进一步分析了1%≤ER<10%组和ER≥10%组患者从辅助内分泌治疗中获益的差别。结果显示,在多变量分析中,171例1%≤ER<10%的患者,辅助内分泌治疗与TTR或OS均无相关性。然而,在1952例ER≥10%的患者,辅助内分泌治疗与更好的TTR(HR,0.24;95%CI,0.16-0.36;P<0.001)和OS(HR,0.32;95%CI,0.2-0.5;P<0.001)相关。
结论
在II-III期HER2阴性的原发浸润性乳腺癌接受新辅助治疗的患者中,ER低表达与更高的pCR率相关。ER表达<10%的患者,更有可能从新辅助化疗中取得pCR,这一cut-off值也是既往ASCO/CAP推荐的。此外,ER≥10%的患者接受辅助内分泌治疗,TTR和OS有更显着的获益。
讨论
临床上,约5%的患者ER表达为1-9%,这是一部分小众群体,很难单独对这一部分人群进行辅助内分泌治疗的临床试验。2015年的St. Gallen专家共识指出,这部分患者是否定义为ER阳性还是有争议的,这部分患者不能单纯仅接受内分泌治疗。这一回顾性研究显示,对于II-III期HER2阴性浸润性乳腺癌,ER<10%的患者与TNBC患者临床特征相似,能从新辅助化疗中取得pCR,且从辅助内分泌治疗的获益较少,提示对于ER<10%的HER2阴性患者可以临床定义为TNBC患者。当然,这一研究仅为回顾性分析,后续还需要更多的研究来进一步证实这一结果。
原始出处:T. Fujii, T. Kogawa, W. Dong, et al. Revisiting the definition of estrogen receptor positivity in HER2-negative primary breast cancer. Ann Oncol mdx397. 24 July 2017.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
38
非常好的文章,学习了,很受益
60
学习了谢谢分享
72
学习谢谢分享
0
学习了不少事情!
78