Cell Reports:PTEN C-端缺失可导致基因组不稳定及肿瘤形成
2014-02-25 佚名 生物通
来自北京大学医学部、康奈尔大学威尔医学院的研究人员证实,PTEN C-端(C-Terminal)缺失可导致基因组不稳定及肿瘤形成。这一研究发现在线发表在2月20日的《Cell Reports》 杂志上。 北京大学医学部尹玉新(Yuxin Yin)教授和康奈尔大学威尔医学院Wen Hong Shen教授是这篇论文的共同通讯作者。尹教授长期从事肿瘤机理研究和抗癌药物机理研
来自北京大学医学部、康奈尔大学威尔医学院的研究人员证实,PTEN C-端(C-Terminal)缺失可导致基因组不稳定及肿瘤形成。这一研究发现在线发表在2月20日的Cell Reports 杂志上。【原文下载】
北京大学医学部尹玉新(Yuxin Yin)教授和康奈尔大学威尔医学院Wen Hong Shen教授是这篇论文的共同通讯作者。尹教授长期从事肿瘤机理研究和抗癌药物机理研究。他是第一个发现抗癌基因p53在细胞周期和基因组稳定性相互作用的人,其研究成果发表在Cell(1992年),引用次数达千次以上。
PTEN基因(磷酸酶基因)是继p53基因后另一个较为广泛地与肿瘤发生关系密切的抑癌基因。PTEN在细胞周期调控及细胞快速生长抑制中起着重要的作用。大量的研究发现在多种类型的癌症中存在PTEN基因突变或缺失。PTEN蛋白的异常表达与癌细胞的生长、凋亡、粘附、迁移、浸润等过程密切相关。
癌症相关PTEN突变被发现散布于整个PTEN基因。PTEN N-端结构域中的磷酸酶功能结构域负责对抗细胞生存和增殖的主要信号通路:PI3 kinase (PI3K)/AKT信号通路。在以往的研究中,尹玉新研究小组证实C端区域是PTEN发挥功能维持染色体完整性的必要条件。PTEN的C-端序列对于其实现核定位以及调控锚定非依赖性生长和细胞迁移极其重要。而大量的突变发生于PTEN的C端,表明这一区域有可能也在肿瘤抑制中起着重要的作用。但C-端的肿瘤抑制功能尚需要确诊的数据确定。
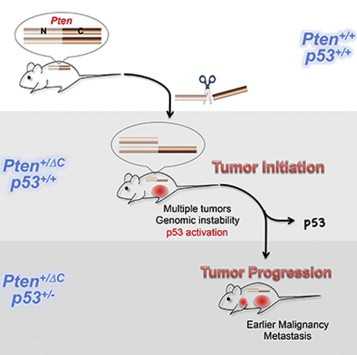
在这篇文章中,研究人员构建出了一种因无义突变导致整个PTEN 蛋白C端区域缺失(Pten△C)的基因敲入(knockin)小鼠模型。他们发现Pten△C杂合子小鼠形成了多种自发性肿瘤,包括一些癌症和B细胞淋巴瘤。PTEN C-端区域杂合缺失也可以导致基因组不稳定以及常见脆性位点重排。研究人员发现PTEN C-端破坏诱导了p53和它的下游靶标活化。同时耗尽p53会促进肿瘤转移但不会影响肿瘤发生,表明p53主要抑制了肿瘤进展。
这些数据证实了Pten C-端在维持基因组稳定和抑制肿瘤形成中发挥了至关重要的作用。
原始出处:
Zhuo Sun1, 2, Chuanxin Huang2, Jinxue He2, Kristy L. Lamb2, Xi Kang1, 2, Tingting Gu2, Wen Hong Shen2and Yuxin Yin1, 2.PTEN C-Terminal Deletion Causes Genomic Instability and Tumor Development.Cell Reports, 20 February 2014 doi:10.1016/j.celrep.2014.01.030【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CEL#
30
#肿瘤形成#
29
#Cell#
30
#PTEN#
30