Antioxidants:儿童心脏手术后的氧化应激和脑损伤指标
2022-04-04 从医路漫漫 MedSci原创
儿科心脏手术会引起明显的氧化应激反应。自由基通常与天然的抗氧化剂防御系统处于平衡状态,破坏这种平衡状态会导致DNA、脂质、蛋白质和细胞膜的破坏。
背景:随着外科技术和重症监护医学的最新进展,超过90%的先天性心脏病(CHD)儿童患者可以存活到成年。这一不断增长的人口面临的最普遍的疾病之一是神经认知障碍。虽然出生前和出生后的几个因素影响神经功能,但婴儿时期的心脏手术已被证明影响未成熟大脑的发育。儿科心脏手术会引起明显的氧化应激反应。自由基通常与天然的抗氧化剂防御系统处于平衡状态,破坏这种平衡状态会导致DNA、脂质、蛋白质和细胞膜的破坏。少突胶质细胞谱系中的未成熟细胞稍后将有助于髓鞘形成,它们特别容易受到OS的损伤。鉴于发育中的大脑中存在较高浓度的未成熟少突胶质细胞和脂肪酸,婴儿容易受到OS诱导的损伤。
越来越多的证据表明,儿科患者心脏手术后OS增加,但其与神经损害和总体临床结果的相关性仍不确定。在其他易受伤害的人群中,如早产儿,OS已被证明与较差的神经预后相关。在患有出生窒息的足月儿中,脐带血OS反应与疾病的严重程度相关。此外,据报道,围产期OS水平较高的早产儿在12个月时神经发育较差。考虑到经历出生窒息的足月儿、早产儿和出生时患有CHD的婴儿在脑损伤病理生理学上的相似性,我们假设OS可能在心脏手术周围的神经功能障碍中发挥作用。在这项前瞻性研究中,我们试图描述OS的生物标志物尿游离8-异前列腺素F2α(8-iso-PGF-2α)与心脏手术婴儿的临床和神经预后的关系。
目的:儿科心脏手术导致氧化应激(OS)反应增加。在具有相似脑损伤模式的新生儿人群中,OS增加与较差的神经结局相关。我们调查了接受心脏手术的婴儿的OS和脑损伤。
方法:接受或不接受体外循环(CPB)心脏手术的6个月或以下的患者被纳入这项前瞻性的观察性研究。将患者分为婴儿组(30天~6个月)和新生儿组(<30天)进行分析。分别于术前、术后0h和术后2 4h测定尿OS生物标志物8-异前列腺素F2α(8-iso-PGF-2α)。分别于术前、术后0、72h检测血清脑损伤标志物S100B蛋白。对手术中的幅度积分脑电进行分析。使用Bayley III或Vinland测试对所有患者在24个月大时进行神经心理评估。
结果:纳入62名患者,其中44人接受了随访神经学评估。术后8-isPGF2α和S100B水平升高。术后S100B水平与术后24 h 8-iso-PGF_2α水平呈正相关(Rho=0.5224;p=0.0261)。术后即刻8-iso-PGF-2α水平与术中癫痫发作负担呈正相关(Rho=0.4285,p=0.0205)。神经学评估异常的患者术后72小时S100B水平升高(p=0.048)。术后24小时8-iso-PGF-2α水平也与神经功能异常有关。
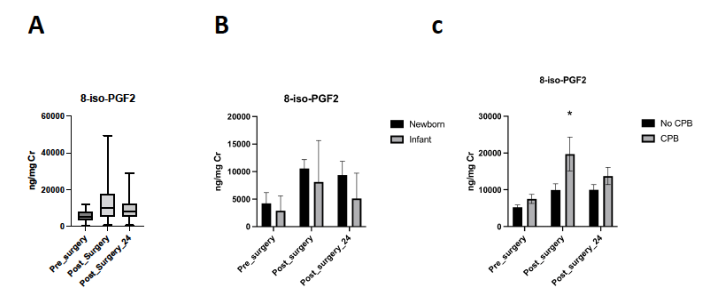
图1 8-iso-PGF-2α的水平。(A)8-iso-PGF_2α在围手术期的演变。(B)考虑年龄组的围手术期8-iso-PGF-2α水平。(3)考虑术中体外循环的需要,围术期8-iso-PGF-2α的变化。(*p=0.0214)

图2 S100B蛋白的水平。(A)S100B蛋白在围手术期的演变。(B)S100B蛋白水平取决于手术期间是否有电除颤

图3 术后即刻S100B水平与术后24小时8-iso-PGF-2α水平的相关性
表1 使用贝利婴幼儿发育量表(贝利-III)的神经发育结果。


图4 S100B在72小时水平的ROC曲线。
结论:儿科心脏手术后8-iso-PGF-2α水平与脑损伤的几个指标相关,包括脑损伤生物标记物、术中癫痫发作和随访中的异常神经评估,表明氧化应激反应在这一人群脑损伤的起源中具有重要意义。
原文出处:
Cañizo Vázquez D, Hadley SM, Pérez Ordóñez M, et al.Oxidative Stress and Indicators of Brain Damage Following Pediatric Heart Surgery.Antioxidants (Basel) 2022 Feb 28;11(3)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#损伤#
31
#应激#
45
不错
52
好文章,值得一读。
55