European Radiology:舟骨韧带撕裂患者的影像学评估:定量评估的选哪个?
2022-04-14 shaosai MedSci原创
舟骨背侧移位(SDD)目前是舟骨不稳定患者的负面预后因素,常提示需进一步的手术治疗。

舟骨不稳定(SLI)的诊断在临床上具有挑战性,舟骨骨间韧带(SLIL)的损伤是产生舟骨不稳定的主要因素之一。舟骨背侧移位(SDD)是一个重要的诊断因素,但其评估的标准至今没有明确的指南。同时,SDD目前是舟骨不稳定患者的负面预后因素,常提示需进一步的手术治疗。此外,以往的研究表明,SDD 的程度与舟骨不稳定的严重程度和骨关节炎的存在相关。因此,建立一个可靠的评估SDD的定量成像方法十分重要。
Chan等学者使用标准X线片对20名患者进行研究,结果证实使用背侧切线(DTL)方法最为实用,且可靠性较高。然而,X线片很容易受到病人定位问题的影响,对识别早期腕关节不稳定的敏感性较低。因此,Teixeira等学者提出在CT图像上测量桡骨后角(PRSA)进行评估,定义为舟骨窝表面平面与舟骨最后点之间的角度。Meister等学者指出,定义为矢状面MR图像上SDD相对于桡骨关节面的比率的放射状舟骨同位率(RSCR)与SLIL撕裂呈正相关。
近日,发表在European Radiology杂志的一项研究比较了四种不同的SDD定量评估方法(传统X线片上的DTL,CT和MR上的PRSA,以及MR上的RSCR),每种方法得到的数值都与SLIL撕裂和腕关节软骨病(舟骨高级塌陷(SLAC))进行相关性分析,为进一步优化和规范背侧舟骨脱位的成像评估提供了数据支持。
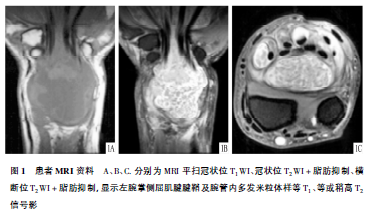
本项研究前瞻性地纳入160名连续接受CT关节造影检查以评估疑似舟骨韧带撕裂的患者。其中65名患者的MR图像可用。两位阅读者使用背切线(DTL)方法独立评估了常规X线片上的舟骨位移,CT和MR上的桡骨后角(PRSA)以及MR上的桡骨同位比。这些测量结果在有和没有舟骨韧带撕裂的患者组中进行了比较。
CT上的DTL和PRSA的测量结果优秀(ICC=0.93和0.88),MR上的PRSA良好(ICC=0.65),而RSCR为中等(ICC=0.49)。在正常和破裂的SLIL患者之间,CT上的DTL和PRSA值有明显增加(P < 0.0001)。基于MR的方法也有同样的趋势,但这些差异只在一个阅读者中有意义。唯一能区分正常和部分破裂的SLIL患者的方法是CT上的PRSA。CT上的PRSA对SLIL破裂的诊断效果最好(敏感性和特异性为70-82%和70-72%)。

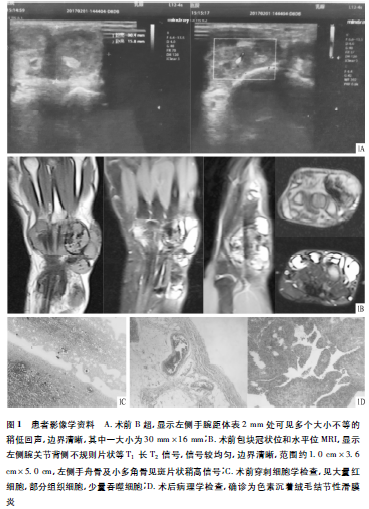
图 a, b 轴位和冠位CT关节造影图像,显示了舟骨背侧部分的撕裂(脂肪箭头)。 c, d 两位读者认为背侧切线(c)是正常的(-0.5和-1.1毫米),而CT上两位读者认为桡骨头后角(d)是异常的(105°和112°)
本研究表明,对于SDD的定量评估,标准X线片上的DTL和CT上的PRSA是最一致的成像指标,具有很好的观察者间可重复性,异常值与CT关节造影上的SLIL撕裂和软骨病变密切相关。CT上的PRSA是唯一可以区分CT关节造影上正常和部分撕裂的SLIL患者的方法。两种被评估的基于MR的方法的观察者之间的可重复性都很好,但与CT关节造影结果的相关性较差。
原文出处:
Pedro Augusto Gondim Teixeira,Kamel Rouizi,Patrice Moustache-Espinola,et al.Imaging assessment of dorsal scaphoid displacement in patients with scapholunate ligament tears: what is the best option for quantitative assessment?.DOI:10.1007/s00330-021-08446-z
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
32
#定量评估#
55
#韧带#
43
#影像学评估#
47