Chest:危重成人视频喉镜气管插管效果如何?
2017-06-23 xing.T MedSci原创
由此可见,VL技术并没有提高ICU患者气管插管的首次成功率,相比于DL。这些发现不支持ICU患者常规使用VL。
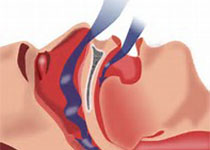
重症监护病房(ICU)患者进行气管插管与导致危及生命的不良事件的风险增加有关,因为病情不稳定、迅速恶化、准备时间有限和操作者专业知识有所不同。近日,呼吸领域权威杂志chest上发表了一篇荟萃分析文章,研究人员旨在比较ICU中需要进行气管插管的患者采用视频喉镜(VL)和直接喉镜(DL)的效果。
研究人员检索了PubMed、Embase和Cochrane数据库中相关研究,检索时间从成立只时到2017年1月30日。研究人员将报告了采用VL和DL进行气管插管的ICU患者出现任何预先定义的结局数据的随机对照试验(RCT)纳入分析。结果采用风险比(RR)或平均差异(MD),并伴有95%可信区间(CI)来表示。
该荟萃分析共纳入了5篇RCT,包括1301例患者。尽管采用VL改善了声门可视化情况(RR=1.24;95%CI为1.07-1.43;P=0.003),但使用VL并没有导致第一次尝试的成功率显著增加(RR=1.08;95%CI为0.92-1.26;P=0.35),与DL相比。此外,气管插管时间(MD=4.12秒;95%CI为-15.86至24.09;P=0.69)、困难插管(RR=0.72,95%CI为0.30-1.70;P=0.45)、死亡率(RR=1.02,95%CI为0.84-1.25;P=0.83)以及其他大多数并发症在VL和DL组之间较为相似。
由此可见,VL技术并没有提高ICU患者气管插管的首次成功率,相比于DL。这些发现不支持ICU患者常规使用VL。
原始出处:
Hui-Bin Huang,et al. Video Laryngoscopy for Endotracheal Intubation of Critically Ill Adults: A Systemic Review and Meta-analysis.chest.2017. http://journal.publications.chestnet.org/article.aspx?articleid=2634649
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Chest#
24
#EST#
31
学习了,谢谢分享!
55
#气管插管#
30
技术好了用不用视频引导都一样?
63