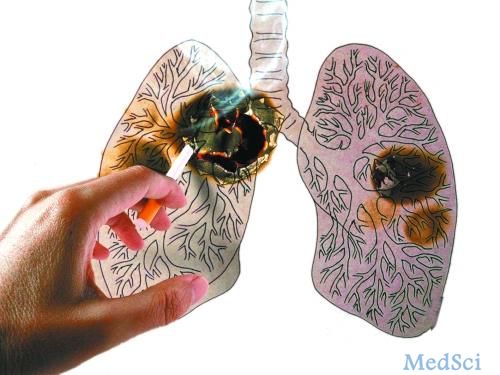
Plos One:非小细胞肺癌患者的EGFR突变比例与TKI治疗密切相关!
2017-05-20 MedSci MedSci原创
分析表皮生长因子受体(EGFR)可以评估非小细胞肺癌(NSCLC)患者对酪氨酸激酶抑制剂(TKIs)治疗的反应性。目前,以及在肺癌中观察到肿瘤内分子异质性的存在。近期,一项发表在杂志Plos One的研究旨在评估肿瘤样品中突变的肿瘤细胞的百分比是否会影响对TKIs治疗的反应。此项研究使用下一代测序仪,共分析了931例NSCLC患者的EGFR突变状态(外显子18,19,20,21)。在将下一代测序仪
分析表皮生长因子受体(EGFR)可以评估非小细胞肺癌(NSCLC)患者对酪氨酸激酶抑制剂(TKIs)治疗的反应性。目前,以及在肺癌中观察到肿瘤内分子异质性的存在。
近期,一项发表在杂志Plos One的研究旨在评估肿瘤样品中突变的肿瘤细胞的百分比是否会影响对TKIs治疗的反应。
此项研究使用下一代测序仪,共分析了931例NSCLC患者的EGFR突变状态(外显子18,19,20,21)。在将下一代测序仪分析后获得的突变等位基因的百分比与每个肿瘤中的肿瘤细胞百分率进行标准化之后,计算突变的肿瘤细胞的百分数。
此项研究结果显示:下一代测序共发现了167个样品中有EGFR突变(17.9%),主要是外显子19的缺失。在18例接受TKI治疗的患者随访中,突变型肿瘤细胞百分比与临床反应有显着相关性(P = 0.017)。与突变型肿瘤细胞率低于56%(8.2个月)的患者相比,具有超过56%的突变型肿瘤细胞百分比的患者具有较高的总体存活率(26.3个月),结果具有统计学趋势(P = 0.081)。
此项研究表明:肿瘤中EGFR突变的肿瘤细胞的百分比与TKIs的治疗反应相关。EGFR突变状态的“定量结果”可能提供有用的信息,以便识别那些可能受益于TKI的患者。
原始出处:
de Biase D, Genestreti G, et al. The percentage of Epidermal Growth Factor Receptor (EGFR)-mutated neoplastic cells correlates to response to tyrosine kinase inhibitors in lung adenocarcinoma. PLoS One. 2017 May 16;12(5):e0177822. doi: 10.1371/journal.pone.0177822. eCollection 2017.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非小细胞#
41
#Plos one#
44
#肺癌患者#
33
好文,值得点赞!认真学习,应用于实践!谢谢分享给广大同好!
71
好好学习
72
#TKI#
33
#GFR#
33
#非小细胞肺癌患者#
36
每天学习一点新知识谢谢了
66
疗效好的,容易发生突变
68