前列腺癌家族史是前列腺癌的一个公认的风险因素,在一级亲属男性中,风险大约增加2至3倍。乳腺癌的一级家族史也是前列腺癌的一个风险因素,有前列腺癌家族史的女性在绝经后乳腺癌的风险也会增加。最近的报告显示,胰腺癌和卵巢癌中也发存在上述趋势,支持了激素敏感型癌症的共同遗传倾向。

在普通人群中,有癌症家族史的患高级别前列腺癌的风险已有描述,但在一个选择进行前列腺活检男性的国际队列中还没有描述。
近期,来自美国的研究人员在《Eur Urol》上发表文章,他们根据癌症家族史评估了活检时发生高级别前列腺癌的风险。
这是一项多中心研究,研究对象是2006年至2019年接受前列腺活检的男性,包括北美和欧洲的12个站点。所有站点都记录了一级前列腺癌家族史;四个站点包括了更详细的受影响亲属数量、患有前列腺癌的二级亲属和乳腺癌家族史数据。研究人员使用多变量逻辑回归评估了高等级(Gleason等级组≥2)前列腺癌的几率。对家族史的定义进行了单独的模型拟合,包括了一级和二级前列腺癌和乳腺癌家族史。
共有15799名男性有一级前列腺癌家族史,4617名有更详细的家族史(中位年龄65岁,两个队列)。一级前列腺癌的调整后几率是1.77(95%置信区间[CI]1.57-2.00,P<0.001,风险比[RR]=1.40),二级前列腺癌的调整后几率是1.38(95%CI 1.07-1.77,P=0.011,RR=1.22),一级乳腺癌家族史的调整几率是1.30(95%CI 1.01-1.67,P=0.040,RR=1.18)。交互项显示,家族史的影响在前列腺特异性抗原上没有差异,但在年龄上有差异。这项研究因种族和先前阴性活检数据的缺失而受到限制。
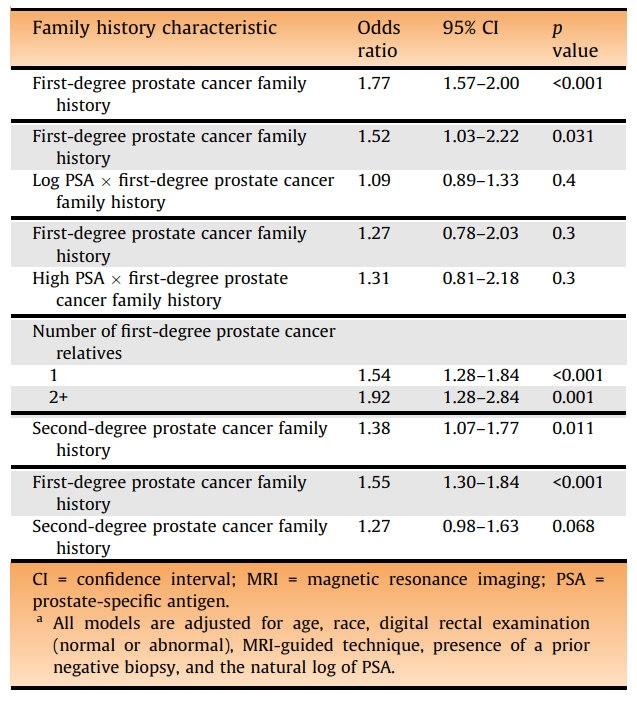
多变量逻辑回归模型评估高等级前列腺癌风险
综上所述,对有活检适应症和有前列腺或乳腺癌家族史的男性,他们的高级别前列腺癌风险有一定程度的增加,且与其他风险因素无关。
原始出处:
Matthew B Clements , Emily A Vertosick , Lourdes Guerrios-Rivera et al. Defining the Impact of Family History on Detection of High-grade Prostate Cancer in a Large Multi-institutional Cohort. Eur Urol. Dec 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#前列腺癌风险#
0
#癌风险#
44
#家族史#
53
学习了
44