JAMA Netw Open:绝经前妇女乳腺癌家族史与乳腺密度有关吗?
2022-02-24 MedSci原创 MedSci原创
绝经前妇女的FHBC与乳房X线密度呈正相关。本研究结果强调了乳腺密度的遗传因素,以及对有乳腺癌家族史的绝经前妇女进行年度筛查的必要性。
一级亲属(母亲、姐妹)中有乳腺癌(FHBC)阳性家族史的女性患乳腺癌的风险增加2到4倍。乳房X光片上的高密度乳房也会增加患乳腺癌的风险。乳腺密度超过75%的女性患乳腺癌的风险是密度低于5%的女性的4到6倍。绝经前女性的乳房密度比绝经后女性高,因为乳房X光密度随着年龄的增长缓慢下降。
简单来说,乳腺癌家族史(FHBC)和乳腺x线片显示的乳腺密度是乳腺癌的独立危险因素,但FHBC和绝经前妇女乳腺密度之间的关系尚不清楚。本研究通过定量和定性的方法研究绝经前妇女FHBC与乳腺密度的关系。
这项单中心队列研究调查了两个回顾性队列:375名绝经前妇女的发现组和14040名绝经前妇女的验证组。发现组的女性数据收集于2015年12月至2016年10月之间,验证组的女性数据收集于2010年6月至2015年12月之间。数据分析时间为2018年6月至2020年6月。
主要结果是使用Volpara(发现集)和BI-RADS(乳腺成像报告和数据系统)乳腺密度(验证集)对乳腺密度进行定量测量,以体积百分比密度表示。对发现集使用对数变换正态分布,对验证集使用逻辑分布,进行多变量回归。
研究结果显示,在纳入研究的14415名绝经前女性中,发现集和验证集具有相似的特征。在发现集中,与没有FHBC的参与者相比,患有FHBC的参与者更可能具有更高的平均密度体积百分比(11.1%对9.0%)。在多变量调整模型中,患有FHBC的女性的体积百分比密度比没有FHBC的女性高25%;有1名受影响亲属的女性高出24%,但与没有受影响亲属的女性相比,至少有2名受影响亲属的女性高出24%。
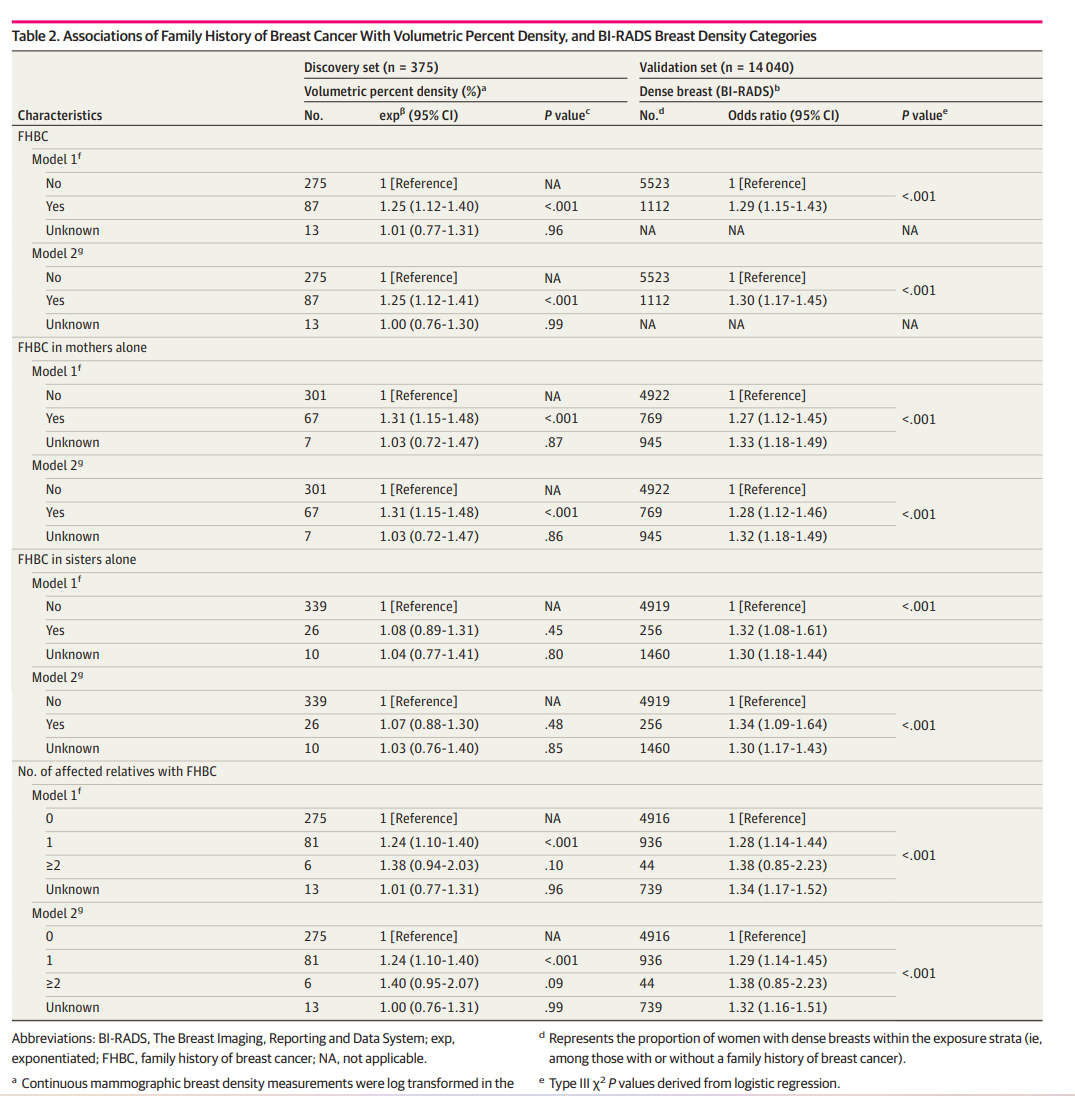
乳腺癌家族史、密度体积百分比和BI-RADS乳腺密度类别的关系
在验证数据集中,与无FHBC的女性相比,FHBC阳性的女性更可能有高密度乳房(BI-RADS 3-4)。在多变量调整模型中,与未患FHBC的女性相比,患有FHBC的女性拥有高密度乳房(BI-RADS 3-4)的几率高出30%;有1名受影响亲属的女性高出29%,但与没有受影响亲属的女性相比,至少有2名受影响亲属的女性高出29%。
总之,在这项队列研究中,绝经前妇女的FHBC与乳房X线密度呈正相关。本研究结果强调了乳腺密度的遗传因素,以及对有乳腺癌家族史的绝经前妇女进行年度筛查的必要性。
参考文献:Han Y, Moore JX, Colditz GA, Toriola AT. Family History of Breast Cancer and Mammographic Breast Density in Premenopausal Women. JAMA Netw Open. 2022;5(2):e2148983. doi:10.1001/jamanetworkopen.2021.48983
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#NET#
37
#PE#
45
#绝经前#
32
#绝经#
41
#乳腺密度#
50
#家族史#
41