继CAR-T之后,TCR技术或成为第3代免疫疗法明星
2017-07-13 医麦客 医麦客
YUGDRyoXo3aAqYbNGLLng1TUQbUq1k3qPB6tm8atROxqFD5suUKF55d4uE5tOgbPyJLn069l0wJlnr0iC4Kg4MDBg44oMRjh3ke3DGRiIDggHvx5M3L7xHk0gQF4d0jeJBd/vkelITAwHvuKeDaJT6U5x8PQEgCQX4HJMBbIQsswIgQQhiSoH8ARiKBAQbsh1ghCAQAw
美国时间7月3日,全球领先的TCR公司Immunocore宣布其合作伙伴葛兰素史克(GSK)又开展了一项计划作为他们正在进行的肿瘤免疫疗法合作的一部分,该合作于2013年首次推出,是基于Immunocore公司的T细胞受体(TCR)平台ImmTAC,该平台承诺创造更小的生物分子,从而达到常规单克隆抗体无法达到的目标,是Immunocore公司的核心技术。

Immunocore(图片来源 businessmag.co.uk)
作为全球领先的TCR公司Immunocore,在检查点抑制剂PD-1/PD-L1(如默克的Keytruda、BMS的Opdivo等)已获批上市,诺华和Kite公司的首例CAR-T疗法也预期于2017年底/ 2018年初将获得批准之际,Immunocore牵手GSK,希望可以证明TCR技术是免疫肿瘤学药物的“第三代”明星。
Immunocore是一家总部位于英国的生物技术公司,成立于2008年,于2015年获得3.2亿美元投资,为近年来欧洲生物技术公司最大的融资。其核心技术为基于T cell receptor (TCR)改造的ImmTAC平台,而这项技术更是得到了众多大型制药公司的青睐,目前Immunocore已与阿斯利康、基因泰克、葛兰素史克以及礼来等公司达成了广泛的合作。

Immunocore的合作伙伴(图片来源 Immunocore官网)
那ImmTAC 到底有何过人之处呢?
竟然能够在众多技术中脱颖而出。
ImmTAC技术原理
ImmTAC(Immune mobilisingmonoclonal TCRs Against Cancer,字面上我们可以理解为抗肿瘤免疫激动单克隆T细胞受体)本质上属于一类新型的双特异性生物大分子,是由工程化改造的T细胞受体(T cellreceptor, TCR)以及抗CD3的scFv组成。
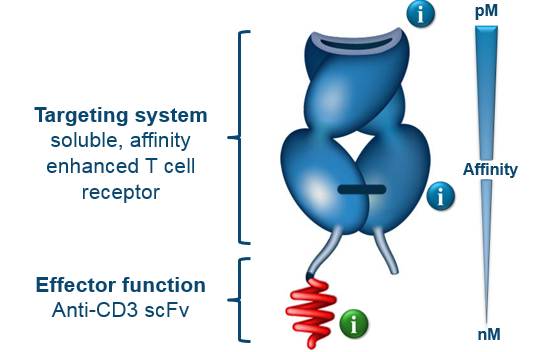
ImmTAC结构(图片来源Immunocore官网)
在本质上,识别癌症抗原的TCR对其相应的抗原的亲和力通常很低,这就味着癌细胞对免疫系统基本上是不可见的,这一问题进一步加剧了癌细胞对pHLA的调控。
所以为了解决个问题,ImmTAC使用了工程改造的TCR为基础的靶向系统。TCR识别细胞内抗原,处理并递呈到细胞表面,形成peptide-HLA复合物(pHLA)。通过噬菌体展示技术(phage display process)显著提高了TCR的亲和力,比抗原抗体结合的亲和还要高出9倍左右,这种高亲和力识别意味着ImmTAC分子可以有效地识别肿瘤细胞表面的pHLA。而且目前世界上具备获得高亲和力TCR的公司只有Immunocore公司(PM级)。除了TCR,抗CD3的scFv则负责吸引、招募T细胞至肿瘤细胞周围并激活T细胞发挥肿瘤的杀伤作用。
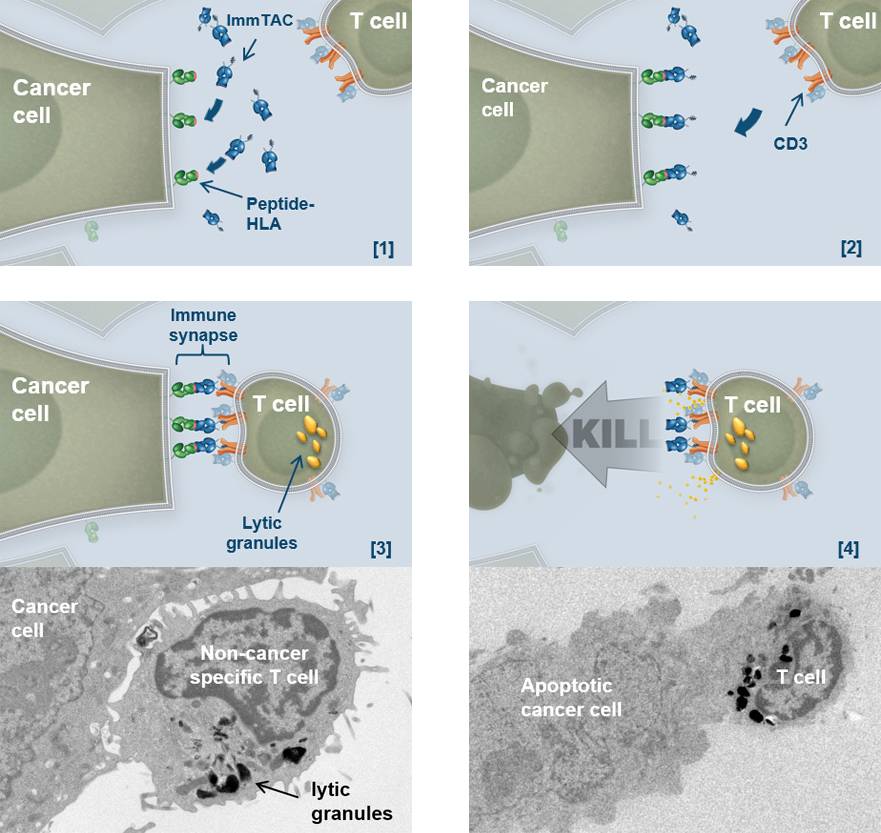
ImmTAC肿瘤杀伤示意图(图片来源 Immunocore官网)
如上图,ImmTAC分子的工作原理:
1、ImmTAC分子识别并与肿瘤细胞表面的pHLA强烈结合
2、ImmTAC分子的自由端(抗CD3抗体片段)招募或重定向循环T细胞到肿瘤部位
3、ImmTAC分子在癌细胞和T细胞之间形成桥梁,能够形成完美优化的免疫突触
4、重新定向和激活的T细胞释放溶解性颗粒,从而杀死癌细胞
下面的视频显示了ImmTAC重定向T细胞杀死的真正的癌细胞的过程,另一张原理图显示了每个视频中可以看到的不同细胞类型。
ImmTAC重定向非癌特异性T细胞(以蓝色显示)杀死癌细胞(以红色显示),同时使相邻的非癌细胞(以绿色显示)完好无损。(图片来源 Immunocore官网)
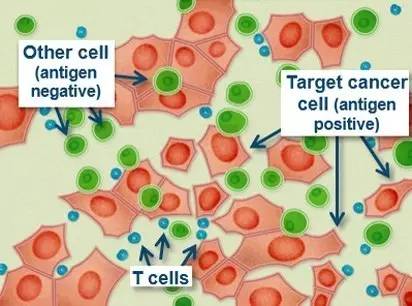
不同的细胞类型(图片来源 Immunocore官网)
一个单独的ImmTAC重定向非癌症特异性T细胞(蓝色显示)杀死了多个癌细胞(红色表示)。(图片来源 Immunocore官网)
不同的细胞类型(图片来源 Immunocore官网)
应用ImmTAC技术的其他研发管线
基于此项技术,Immunocore公司的产品线有超过10种在研药物,且大多应用于肿瘤的治疗。
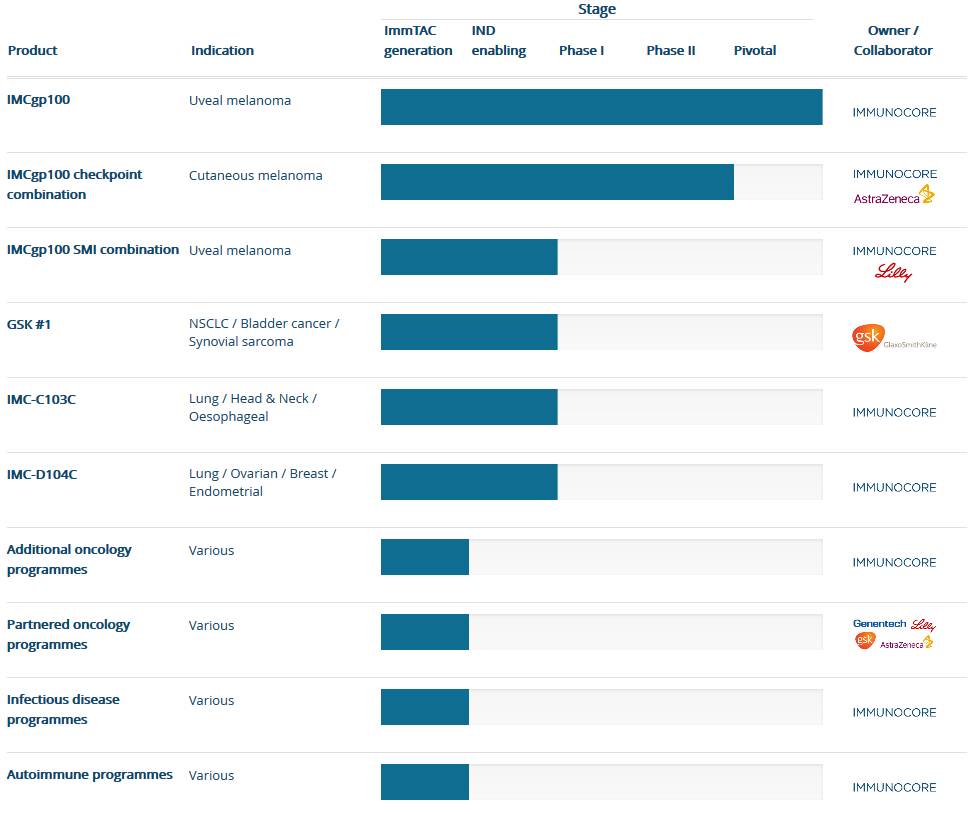
研发管线(图片来源 Immunocore官网)
核心产品IMCgp100临床最新进展
目前进展最快的为治疗葡萄膜黑色素瘤的IMCgp100,该产品是靶向肿瘤特异性的gp100多肽的TCR和抗CD3的scFv组成的双特异性蛋白,目前已经进入临床试验的关键性研究阶段(Pivotal),美国FDA已经授予了IMCgp100用于治疗葡萄膜黑素瘤的孤儿药资格认定。除了单药治疗之外,IMCgp100联合durvalumab(阿斯利康PD-L1抗体)以及IMCgp100联合 tremelimumab(阿斯利康CLTA-4 抗体)的临床研究也处在第二阶段。
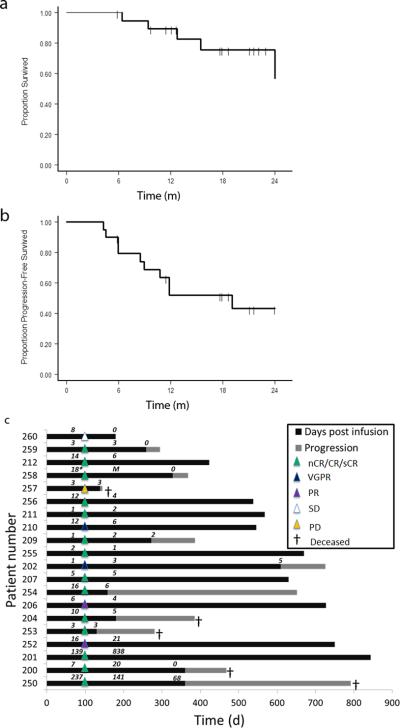
在2017年ASCO年会上,Immunocore公司公布了IMCgp100的一项临床结果,在患者内剂量升高的I期研究中,招募了19名转移性葡萄膜黑色素瘤患者,并显示了5.6个月的中位无进展生存期(PFS),相比较之前报道的2.6-2.8个月的中位PFS是具有优势的。在24周(6个月)的PFS率为57%,而先前的临床研究中报道的数据仅为19-27%。
基于IMCgp100在转移性葡萄膜黑色素瘤患者中的有希望的临床数据,Immunocore正在启动一项关键试验,以推进IMCgp100向商业化发展。另外,Immunocore正在就一系列其他高发型肿瘤进行靶点开发,从而即将打开更广阔的适应症前景。同时Immunocore还在积极寻求与其他抗肿瘤免疫药物的联合使用。这项令人大开眼界先进技术是否能成功转化为医学奇迹,满足更多亟待满足的患者需求?我们拭目以待。
结语
在肿瘤免疫治疗大行其道的今天,PD-1/ PD-L1抗体已经多到满天飞了,自带光环的CAR-T疗法也即将走向上市。所以在现阶段,扎堆研发此类疗法的现象尤为严重,而Immunocore公司算是肿瘤免疫治疗领域的一股清流了。
从理论上来讲,ImmTAC技术要比PD-1/PD-L1抗体更具有优势。PD-1/PD-L1有较高的毒副作用、缺乏肿瘤靶向特异性以及较低的响应率等缺点。而ImmTAC技术平台通过特异性高亲和力的TCR,能够识别肿瘤特异性抗原,并招募激活T细胞发挥细胞杀伤作用,具有更好的特异性和安全性。
而且相比较CAR-T疗法而言,针对实体瘤则是一大优势,但同时TCR也要求更高的技术水平来突破高壁垒。当然,客观上来说,要成为下一代免疫疗法新星,Immunocore还有很长的路要走。
参考出处:
https://pharmaphorum.com/news/immunocore-gsk-pick-third-cancer-immunotherapy-target/
http://www.immunocore.com/technology/immtac-molecules-in-action
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#CAR-#
26
学习
62
学习
76
学习
52
学习了
67
学习
56
#TCR#
36
学习
26
TCRT细胞受体
27
赞赞赞
26