CSC&OCC 2015:胡盛寿:心力衰竭外科治疗——挑战与突破
2015-09-14 MedSci MedSci原创
本文作者:北京阜外心血管病医院院长,中国工程院院士,美国心脏病学院会员胡盛寿。心力衰竭是一种全球性疾病,欧洲有超过1000万,美国超过580万,中国超过500万人患有心力衰竭。30-65岁人群发病率为1.5-2.0%,65岁以上人群发病率为6-10%。心力衰竭是全球吃唯一呈增长趋势的心脏疾病,是心血管病领域未来要面临的巨大挑战。2003年,对中国10省市20个城区和农村15518人口调查显示,心衰
本文作者:北京阜外心血管病医院院长,中国工程院院士,美国心脏病学院会员胡盛寿。

心力衰竭是一种全球性疾病,欧洲有超过1000万,美国超过580万,中国超过500万人患有心力衰竭。30-65岁人群发病率为1.5-2.0%,65岁以上人群发病率为6-10%。心力衰竭是全球唯一呈增长趋势的心脏疾病,是心血管病领域未来要面临的巨大挑战。
2003年,对中国10省市20个城区和农村15518人口调查显示,心衰的发病率女性为1.0%,男性为0.7%,35-74岁人群患病率为0.9%。对1993-2007年住院心衰患者病因分析,有45%是冠心病患者,38.7%为高血压患者,其余主要的病因还包括糖尿病和风湿性心脏病。且随着年龄增加,冠心病和高血压发生率增加,扩张心肌病和瓣膜病发生率下降。
关于心衰药物的研究近20年来没有重大进展,现有分子靶点和信号通路药物不能逆转心衰重构。外科干预成为心力衰竭救治很重要的方法。
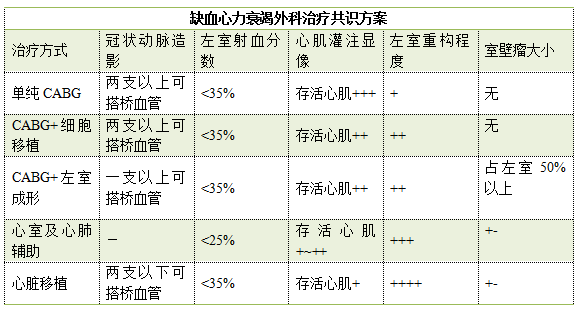
心力衰竭目前的外科治疗手段主要包括:
-心肌血运重建术
-二尖瓣成形术
-干细胞移植
-大网膜+心耳包裹术
-左心室成形术
-可注射生物胶
-机械辅助循环
-心脏移植术
一、常规CABG术
一项6665例搭桥手术临床研究证实非体外循环搭桥使患者短期获益,重症患者体外循环下CABG更加有利。发表于NEJM上一项研究显示,重病患者非体外CABG无特殊获益。
对于血管条件适于血运重建、有存活心肌、无室壁瘤、LVEF低于40%、轻度左室重构患者,采用单纯CABG可获得比其它治疗方式更好的临床结果。
二、CABG+二尖瓣成形术
调查2005-2013年1542例同期接受瓣膜术患者,平均随访3年。结果表明,患者围术期死亡率2.5%。说明CABG+二尖瓣成形术能够有效改善心功能,长期预后良好。
三、CABG+细胞移植
细胞移植是未来心衰救治很重要的一个方向,但由于伦理学原则和生物安全性原则,细胞移植来源细胞受到很大限制。阜外医院开展了患者自体骨髓来源单个核细胞经桥血管移植随机对照双盲临床研究,取得了良好的效果。该研究结果发表在2011的JACC杂志,被2013版ACC/AHA心衰治疗指南引用。
四、CABG+心耳组织块+大网膜包裹术
CABG+心耳组织块+大网膜包裹术作为危重症冠心病治疗的新术式,并未增加手术风险和围术期并发症,因此该术式安全可行。其有效性有待Phase II临床试验证实。
五、CABG+心室成形
心室成形术是治疗合并室壁瘤的心衰的重要外科手段。阜外医院采取改良内膜还缩术治疗145例该类患者,MRI结果证实心内膜环缩可更好地恢复心脏几何结构和功能,与传统线性缝合相比,不良反应发生率和再住院率降低。CABG+左室成型具有良好的远期生活质量和存活率。
六、可注射生物凝胶治疗心衰
2015年7月,阜外医院开展了国内首例可植入海藻酸盐凝胶治疗扩张型心肌病合并二尖瓣、三尖瓣中度关闭不全的心衰患者,术后患者左心室舒张末期内径和射血分数明显改善。
七、心室及心肺辅助
目前治疗心衰的心室辅助技术包括短期心室辅助、心肺辅助和长期心室辅助。阜外医院短期心室辅助和心肺辅助的研究都取得了很好的效果,体外膜肺氧合费用相对较低,适合国人。自2003年起,阜外医院开始进行国产自主心室辅助装置的研发,设计制造的FW-Ⅱ轴流泵于2011年完成了CFDA质检中心检测,获准应用于急性心梗泵衰竭患者,6例患者获得成功应用。
八、心脏移植
随着移植规范时代的到来,我们国家一年心脏移植平均在300~350例。阜外医院从2004年到2013年做了近400例心脏移植,远期生存率国际最高,5年生存率达87.6%。心脏移植是终末期心力衰竭的最终治疗手段,可明显提高远期存活率和生活质量。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#胡盛寿#
41
#CSC&OCC#
44
了解了。。。
95
#OCC#
27