从“黄金搭档”到“金三角”,慢性心衰如何用药物规范治疗?
2016-05-31 MedSci MedSci原创
在“心力衰竭国际学院”2016年第一期会议上,中国医学科学院阜外医院黄晓红教授作了题为《从中国指南看慢性心力衰竭的规范化治疗》的主题报告,其中重点讲到了慢性心衰的药物治疗的各项内容。
在“心力衰竭国际学院”2016年第一期会议上,中国医学科学院阜外医院黄晓红教授作了题为《从中国指南看慢性心力衰竭的规范化治疗》的主题报告,其中重点讲到了慢性心衰的药物治疗的各项内容。

黄晓红教授
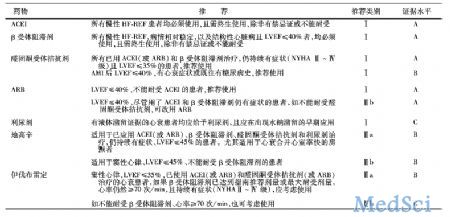
在2014中国心力衰竭诊断和治疗指南中,重点推荐了两类不同等级的药物:
一、可改善预后的药物适用于所有慢性收缩性心衰心功能Ⅱ~Ⅳ级患者
血管紧张素转化酶抑制剂(ACEI)(Ⅰ,A);
β受体阻滞剂(Ⅰ,A);
醛固酮拮抗剂(Ⅰ,A);
血管紧张素受体拮抗剂(ARB)(Ⅰ,A);
伊伐布雷定:用来降低因心衰再住院率(Ⅱa,B),替代用于不能耐受β受体阻滞剂的患(Ⅱb,C)
二、可改善症状的药物推荐应用于所有慢性收缩性心衰心功能Ⅱ~Ⅳ级患者
利尿剂(Ⅰ,C):对慢性心衰病死率和发病率的影响, 并未做过临床研究,但可以减轻气促和水肿,推荐用于有心衰症状和体征,尤其伴显著液体滞留的患者;
地高辛(Ⅱa,B)。
2014中国心力衰竭诊断和治疗指南推荐药物目录
利尿剂:
适应证:有液体潴留证据的所有心衰患者均应给予利尿剂(Ⅰ,C)。
利尿剂包括:噻嗪类、袢利尿剂、潴钾利尿剂、血管加压素受体拮抗剂。指南推荐的剂量如下:
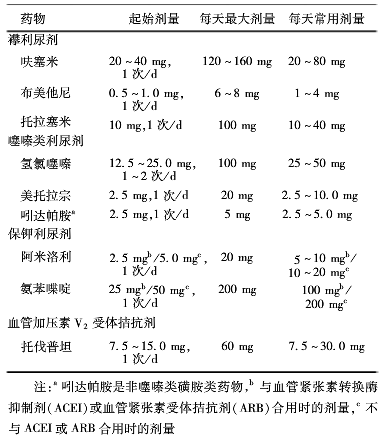
利尿剂的使用可激活内源性神经内分泌系统,特别是RAAS系统和交感神经系统,故应与ACEI或血管紧张素受体拮抗剂(ARB)以及β受体阻滞剂联用。
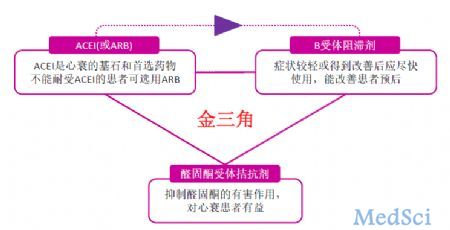
“黄金搭档”:
ACEI和β受体阻滞剂这两种药物被誉为慢性心衰治疗中的“黄金搭档”,两药使用的先后顺序并不重要,重点是尽早合用,能发挥最大的效用,并且可与利尿剂同时开始治疗。
ACEI
ACEI是被证实能降低心衰患者病死率的第一类药物,也是循证医学证据积累最多的药物,是公认的治疗心衰的基石和首选药物,适用于心衰的各个阶段。
适应证:所有LVEF下降的患者必须且终生使用,除非有禁忌症或不耐受(Ⅰ,A)。阶段A为心衰高发危险人群,应考虑使用ACEI预防心衰(Ⅱa,A)。
禁忌证:曾发生致命不良反应,如喉头水肿,严重肾功能衰竭和妊娠妇女。
慎用:双侧肾动脉狭窄,血肌酐>265.2μmol/L(3mg/dL),血钾>5.5mmol/L,伴症状性低血压(收缩压<90mmHg),左心室流出道梗阻(如主动脉瓣狭窄,肥厚型梗阻心肌病)等。
剂量:

应用方法:从小剂量开始,逐渐递增,直至达到目标剂量,一般每隔1-2周剂量倍增1次。滴定剂量及过程需个体化。调整到合适剂量应终生维持使用,避免突然撤药;应监测血压、血钾和肾功能,如果肌酐增高>30%,应减量,如果仍继续升高,应停用。
β受体阻滞剂
适应证:结构性心脏病,伴LVEF下降的无症状心衰患者,无论有无MI,均可应用;有症状和曾经有症状的NYHAⅡ~Ⅲ级,LVEF下降,病情稳定的慢性心衰患者必须终生服,除非有禁忌证或不耐受;
应用方法:推荐用比索洛尔、卡维地洛、缓释琥珀酸美托洛尔,均能改善患者预后。剂量如下:
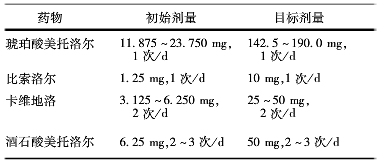
从小剂量开始应用(目标剂量的1/8),逐步增加至靶剂量或最大可耐受剂量(55-60次/min);
避免突然停药,可引起病情恶化。
禁忌证:伴二度及以上房室传导阻滞、活动性哮喘和反应性呼吸道疾病患者禁用。
“金三角”:
醛固酮拮抗剂
由于醛固酮拮抗剂有了改善心衰预后的充分证据,且适应证已扩大到所有伴症状的NYHAⅡ~Ⅳ级心衰患者,加上该药与ACEI联合疗效与安全性均较好,有降低心脏性猝死率证据,因此指南推荐加用醛固酮拮抗剂,与“黄金搭档”组成“金三角”,成为慢性心衰的基本治疗方案。
适应证:NYHA Ⅱ~Ⅳ级且LVEF≤35%的患者;已经使用ACEI(或ARB)和β-B,仍有持续症状(Ⅰ, A);AMI后、LVEF≤40%,有心衰症状或既往有DM史者(Ⅰ,B)。
醛固酮的使用应尽早而广泛,在使用“黄金搭档”后达到目标剂量前就可开始使用。
APB
在“金三角”中,APB在慢性收缩性心衰中并不是首选药,常用于不耐受ACEI的患者。在联用“黄金搭档”后,仍有症状且不耐受醛固酮拮抗剂是,可以用APB来替代醛固酮拮抗剂。
常用的ARB药物及剂量如下:

指南中除了“金三角”与利尿剂之外的两种药
地高辛
适应证:在HF-REF已使用利尿剂、ACEI(或ARB)、β-B和醛固酮拮抗剂、LVEF<45%,仍有持续症状的患者,伴快速心室率的房颤患者尤为合适。(Ⅱa,B)
伊伐布雷定
适应证:适用于窦性心律的HF-REF患者。使用ACEI(或ARB)、β-B和醛固酮拮抗剂,已达推荐剂量或最大耐受量,心率仍>70次/min,并持续有症状(NYHAⅡ~Ⅳ级),可加用伊伐布雷定(IIa,B)。
慢性心衰的药物治疗,虽然许多药物的适用范围都很大,但仍然要在弄清楚病人病情的情况下,按照规范的流程和要求来进行。

慢性心衰药物治疗步骤和流程
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#规范治疗#
48
#金三角#
50
已经收藏了
126
心内都没见过用伊伐布雷定的
141
学习一下!
148
这个不错
116
值得研究
167
黄金搭档
117