Nat Commun:IL-33促进肿瘤微环境的建立并加速胶质瘤的发生发展
2021-12-28 MedSci原创 MedSci原创
胶质母细胞瘤(GBM)是一种高级别神经胶质瘤,尽管目前对于该疾病相关基因组突变情况有了更深入的分子机制研究,但患者的中位总生存期仍仅为14.6个月。
胶质母细胞瘤(GBM)是一种高级别神经胶质瘤,尽管目前对于该疾病相关基因组突变情况有了更深入的分子机制研究,但患者的中位总生存期仍仅为14.6个月。

尽管最大范围手术切除(maximal surgical resection)结合放疗,并同时辅以替莫唑胺(temozolomide)进行辅助化疗的策略在GBM的治疗中取得了一定的进展,但患者的长期存活率还是偏低,其2年和5年的存活率分别维持在25%和10%。
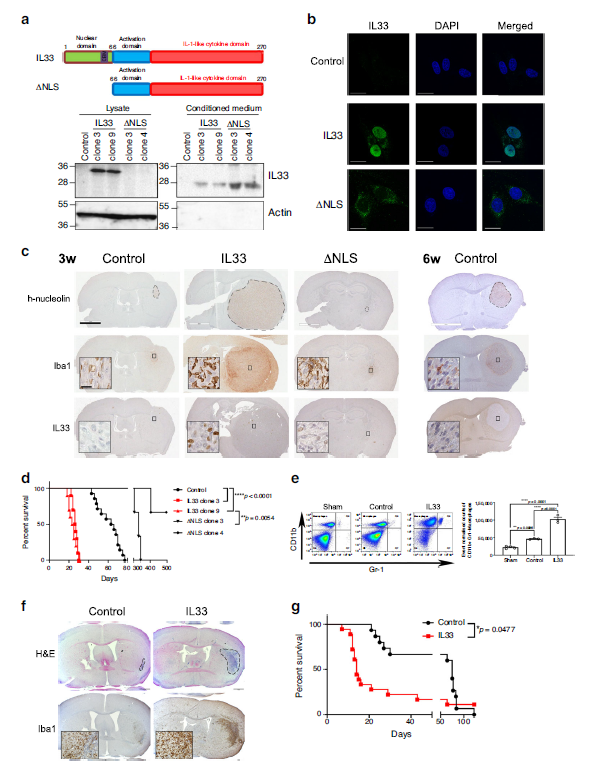
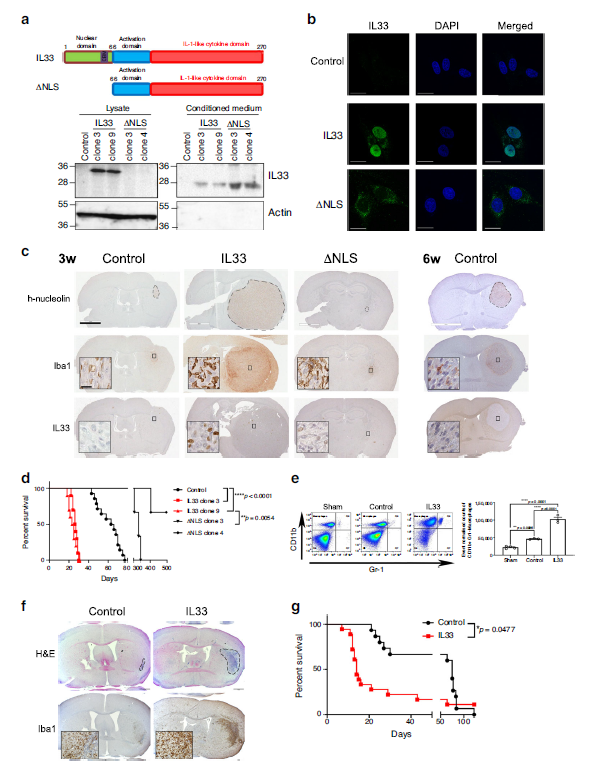 核IL-33是肿瘤生长和巨噬细胞浸润所必需的
核IL-33是肿瘤生长和巨噬细胞浸润所必需的
既往研究显示,巨噬细胞和小胶质细胞的存在会影响胶质母细胞瘤的发生发展并阻止患者产生持久的免疫反应。该研究发现,具有双重功能的细胞因子IL-33能够作为胶质母细胞瘤微环境的调节因子,并促进肿瘤的发生发展。
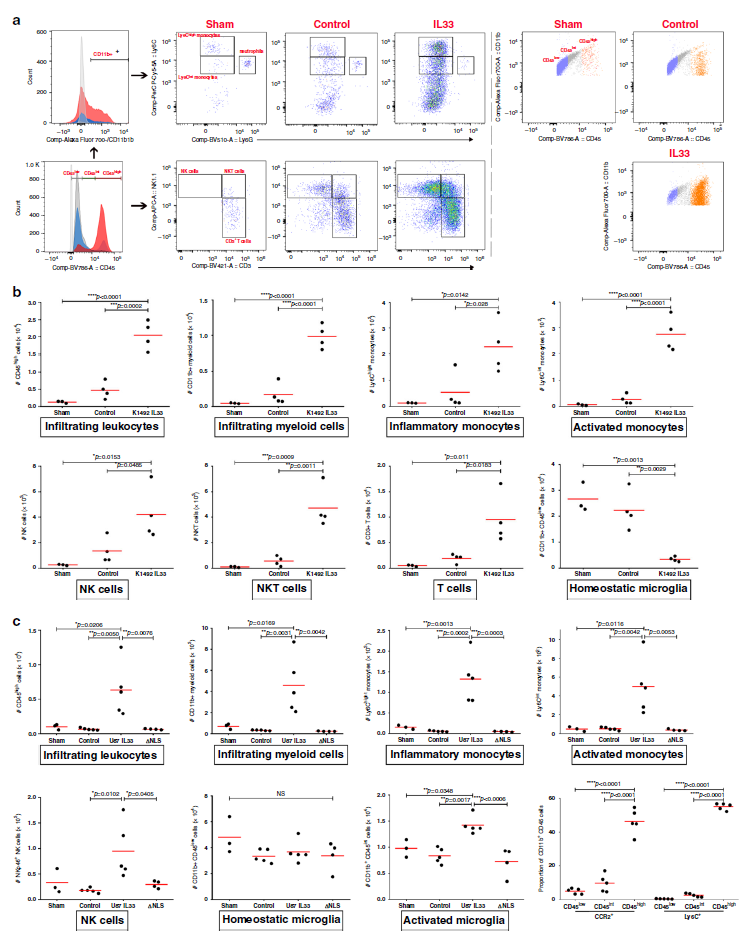
IL-33+胶质瘤与免疫细胞的招募相关
研究人员发现,在大部分的人类神经胶质瘤样本和小鼠模型中,IL-33的表达水平与肿瘤相关的巨噬细胞/单核细胞/小胶质细胞的增多息息相关。此外,核定位和分泌型的IL-33能够调控一些趋化因子,这些趋化因子通过协同招募并激活固有免疫细胞,促进促肿瘤微环境的形成。相反的,核IL-33的缺失会削弱该招募作用,并显著抑制神经胶质瘤的生长,最终提高患者的生存率。
综上,该研究结果揭示了免疫细胞被募集和激活的一个范例,其也为该疾病的治疗提供一种潜在的策略,即将治疗重点不仅放在单独的癌细胞上,也要包括正常的宿主环境。
原始出处:
De Boeck, A., Ahn, B.Y., D’Mello, C. et al. Glioma-derived IL-33 orchestrates an inflammatory brain tumor microenvironment that accelerates glioma progression. Nat Commun 11, 4997 (05 October 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Nat#
33
#发生发展#
52
#COMMUN#
30
#IL-33#
35