盘点:2016颈动脉狭窄全新成果一览
2016-09-24 MedSci MedSci原创
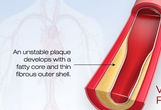
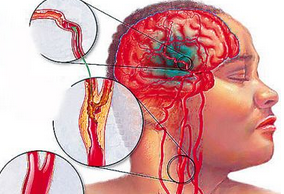
颈动脉是将血液由心脏输送至头、面、颈部的大血管,是脑的主要供血血管之一。据文献报道,重度颈动脉狭窄患者,即便采用有效的药物治疗控制,2年内脑缺血事件发生率也高达26%以上;而60%以上的脑梗塞是由于颈动脉狭窄造成,严重的脑梗塞可导致患者残疾甚至死亡。故而,颈动脉狭窄已经成为当今社会危害人民健康的“头号杀手”之一。【1】Lancet:老年颈动脉狭窄患者,颈动脉内膜切除术优于颈动脉支架成形术在四个
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#新成果#
35
#颈动脉#
34
2016颈动脉狭窄最新成果。
61
颈动脉狭窄最新成果。
72
总结的很好!
63
分享一下!
68
分享一下!
64
2016颈动脉狭窄最新成果一览。
29
分享2016颈动脉狭窄研究成果。
29
很好非常有帮助,谢谢。
23